A Case of Addiction to Heroin and Cocaine
by Siegfried Othmer | September 27th, 2010 The following is a brief report on a recent case of recovery from addiction. This was one of the first addiction cases in which we utilized the extension of our software to cover the low frequency range down to 0.1 mHz (milliHertz). Essentially all of the training of this client took place within this range, i.e. with the exception of several Alpha-Theta sessions. The client has given permission for us to tell her story. She is of middle age now, and has been struggling with addiction to heroin and cocaine for the last fifteen years. When she had her first experience with heroin, she knew immediately that she would do anything to repeat it. The cocaine came later. Episodically, she experienced an overwhelming, compulsive drive to use “that blows everything else away.” She was unable to resist, and in these episodes nothing else mattered. With that lifestyle came going to the bad parts of town, and dealing with people one would rather avoid. “It pulls you into this dark place that makes you hate yourself. It is addiction at its worst.”
The following is a brief report on a recent case of recovery from addiction. This was one of the first addiction cases in which we utilized the extension of our software to cover the low frequency range down to 0.1 mHz (milliHertz). Essentially all of the training of this client took place within this range, i.e. with the exception of several Alpha-Theta sessions. The client has given permission for us to tell her story. She is of middle age now, and has been struggling with addiction to heroin and cocaine for the last fifteen years. When she had her first experience with heroin, she knew immediately that she would do anything to repeat it. The cocaine came later. Episodically, she experienced an overwhelming, compulsive drive to use “that blows everything else away.” She was unable to resist, and in these episodes nothing else mattered. With that lifestyle came going to the bad parts of town, and dealing with people one would rather avoid. “It pulls you into this dark place that makes you hate yourself. It is addiction at its worst.”
Before beginning neurofeedback, she has participated in twenty-five rehabilitation treatments for her addiction over the last fifteen years, and has been through multiple incarcerations related to drug use. She was taking Suboxone, itself an opiate used to detox people from heroin. This helped to manage her heroin addiction and moderate her cravings.
Her early childhood experience is highly relevant here. Even though birth and early development were normal, there was childhood trauma. She began having seizures at age eight, which were attributed to physical insults to the head. The seizures started as petit mal, with the first grand mal seizure at age 11. The seizures are now well-controlled with Keppra. Possibly related to the seizure susceptibility, or to the significant automobile accident she experienced in 2001, she had problems with memory, with impulsivity, and with ongoing depression and anxiety. She could easily slip into a deep depression where life no longer mattered. The anxiety was perpetual. She lived with constant fears and worries.
Other presenting issues included asthma, for which she used an inhaler. There were difficulties with sleep onset, and with frequent waking, for which she took Trazodone. She routinely had frightening dreams. She had headaches monthly, which she brushed off as not much of an issue, and she complained of fatigue during the day. She has had a problem with over-eating in the past, and more recently has struggled with bulimia and anorexia. At the point of coming to neurofeedback, her issue was compulsive over-eating. All these issues notwithstanding, the client is a highly functional person with solid personal relationships and firm career goals.
At the first neurofeedback session, she said that the training “feels really nice.” Her body felt relaxed. She felt “kind of anxious” later after the session. The inter-hemispheric stability protocol was used because of the seizure history. At the second session, the training focused on the right hemisphere, which is preferentially involved in trauma reactions. She felt even calmer and more peaceful, despite some turmoil in her life that had her feeling nervous and shaky coming in. After the session, she reported clearer thinking, and reduced interest in coffee. Over the following sessions, there was a brief increase in asthma severity, which introduced some uncertainty into the proceedings and made the client more hesitant about the training effects. By session seven, however, things were again on a good track, and she decided to start cutting back on some of her medications.
At session fourteen, she reported feeling better in everyday life, not only after sessions. “There has been no urge to use drugs. Pretty shocking, actually. No craving since starting the neurofeedback. I feel like a normal person.” One might wonder why the lack of craving was not reported until the fourteenth session if it had been the case since the first. This is actually quite common in our experience, because it takes someone a while to believe that this is all really happening, and is not ephemeral or transitory.
The review at twenty sessions revealed the following: First of all, the client reports being much more aware of her body. She had been slowly weaning herself off the Soboxone, and was down to the lowest dose before quitting entirely. Trazodone was no longer being used because sleep was much improved, and marked with less scary dreams. Asthma inhaler use was down 50%. A low dose of Cymbalta was changed to Effexor, which she was continuing to take even though she reports her depression to be much improved. “Just getting off the [illegal] drugs is such a great relief. I am much happier.” She reported having good energy during the day. The compulsive over-eating has largely subsided. No recent headaches have been experienced. Seizures remained well-controlled and the Keppra dosage was being maintained.
She was still struggling with some social anxiety, which she was “medicating” with a little alcohol. Her alcohol use had never been problematic, perhaps because she was very sensitive to it. At this point the Alpha-Stim® was introduced to help with the anxiety, and indeed there was an initial strong response.
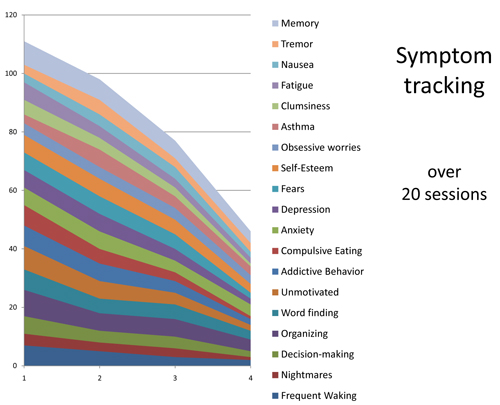
Symptom-tracking data for the first twenty sessions are shown in Figure 1. Symptom severity is scored on a Likert scale of 0-10. The data give no sign of plateauing. On the contrary, progress is actually accelerating, so there is every reason to continue the neurofeedback. At a minimum, gains need to be consolidated. But given such a complex trauma history (both physical and psychological), substantial gains in functionality are in prospect with more extended training. The near-term objectives are the social anxiety and memory issues. The training is ongoing with another therapist who is geographically more convenient.
Alpha-Theta training was introduced during these twenty sessions, but apparently it played only a minor role in the recovery. The client reported experiencing a “busy brain” during these sessions. Even though she reported the sessions as pleasant, there was nothing along the lines of what we consider “deep-state” experiences. In past studies, it was the Alpha-Theta training component that did the heavy lifting in the addictions treatment programs. Here is where the psychological fallout of early trauma experience can be benignly resolved. Here is where many people find their soul. In the present instance, the client was not ready to undertake this work productively, so this part of the journey remains to be undertaken.
The most critical objectives have already been achieved. The client reflected on her experience to date: “Life involved this compulsive, self-destructive drug behavior. It’s gone. The desire for drugs is completely gone.” The work to date has involved no talk therapy, no cognitive re-framing, and no plumbing of the depths of the psyche. There has been nothing but the training of the physiology toward better-regulated function. And when that is accomplished, drug use is no longer part of that life.
In the early days of our work with addictions, at the time of the CRI-Help study in the mid-nineties (Ref. 1), we had become persuaded that recovery from dependency was not contingent on eliminating craving for alcohol or drugs. That is indeed what the data showed. The follow-up reports also demonstrated the importance of continued involvement in the 12-step group process. The two findings are undoubtedly connected. The group process sustained graduates during what remained of the ongoing war with their physiology.
Matters should be different if the infra-low frequency training allows us to eliminate drug craving more systematically and more completely. There is no necessity then to rely on a group process to sustain sobriety. On the other hand, there are issues to be addressed with traditional psychotherapy.
It is tempting to suggest a therapeutic hierarchy in which restoration of physiological functional integrity is paramount at the outset, with emphasis shifting to a psychodynamic process later on. The neurofeedback may very well displace both the detox phase and reliance on cognitive-behavioral methods early in treatment. Neurofeedback is potentially the more organic detox procedure, and it offers more direct access to issues of affect regulation that remain substantially inaccessible to cognitive behavior therapy.
We certainly know how to guide people to states in which the craving for drugs is non-existent. Persistence in such states then becomes progressively reinforced, to the point where it becomes self-sustaining. During the interim period where control is not unequivocal, we must arrange for the continuous availability of neurofeedback. Whenever a person feels himself at risk, neurofeedback must be within proximate reach. This approach could well become the affordable remedy for the vast majority of the addicted population that remains functional within the society and is self-motivated toward recovery. The above case history is representative of that large population.
References
1. Scott WC, Kaiser DA, Othmer S, Sideroff SI. Effects of an EEG Biofeedback Protocol on a Mixed Substance Abusing Population. The American Journal of Drug and Alcohol Abuse, 31:455-469, 2005.
eeginfo.com/research/articles/Biofeedback-Protocol.pdf





