Progress in Remediating PTSD
by Siegfried Othmer | May 27th, 2011 The occasion of Memorial Day 2011 is a good opportunity to reflect on what has been happening in the remediation of PTSD using our latest Infra-Low Frequency (ILF) neurofeedback training. The word breakthrough is over-used, but it does describe the progress that has occurred over the last several years. The most significant event over that time frame was the actual utilization of our methods on a large scale in realistic settings within the military. By now more than 350 service persons have experienced this training at Camp Pendleton, one of six military bases where this work is being conducted. In this fashion, we were able to move from a series of isolated clinical observations in our clinic to a more substantial evaluation in a real-world environment, with independent clinicians guiding the neurofeedback training on the basis of our standard introductory training course, plus the occasional consultation.
The occasion of Memorial Day 2011 is a good opportunity to reflect on what has been happening in the remediation of PTSD using our latest Infra-Low Frequency (ILF) neurofeedback training. The word breakthrough is over-used, but it does describe the progress that has occurred over the last several years. The most significant event over that time frame was the actual utilization of our methods on a large scale in realistic settings within the military. By now more than 350 service persons have experienced this training at Camp Pendleton, one of six military bases where this work is being conducted. In this fashion, we were able to move from a series of isolated clinical observations in our clinic to a more substantial evaluation in a real-world environment, with independent clinicians guiding the neurofeedback training on the basis of our standard introductory training course, plus the occasional consultation.
When neurofeedback is used on such a significant scale, even though it is in a clinical context, certain impressions take hold that rise to the level of accepted fact just as surely as if they had arisen out of a formal research program. For example, it was observed that service persons were more consistent in showing up for neurofeedback training than for any other mental health services on offer for PTSD. It is difficult to see such a finding coming out of formal research, where matters are typically more regimented and prescribed. Another advantage of the real-world setting is that a very broad range of symptom presentations is being encountered, as well as a distribution of symptom severity. This allows a comprehensive set of symptoms to be tracked through the training (on the order of 45 in this case), which would be quite atypical for a research design. An additional advantage was the opportunity to see some of the same persons both before and after deployment, so that impressions could be gained about the durability of the training effects in a combat environment. The clinical environment values the individual case, whereas in research such cases would be submerged in statistical analysis and the richness of detail would be lost.
Yet another observation was that some highly impacted service persons continued to come faithfully for neurofeedback despite the fact that little improvement was noted in the tracking measures. The benefit was apparently more intangible, though clearly still judged to be worthwhile. This is reminiscent of our experience in working with chronic pain. Whereas the specific assessment of pain severity may not budge from the maximal rating, the person’s quality of life may nevertheless be considerably enhanced through the training. And even if the trainee himself may not recognize the benefit, it is not rare that their wives may encourage them to continue, for reasons that may be known only to them.
Finally, in a realistic setting the neurofeedback is imbedded in a larger context of mental health services, so that it does not stand alone. This would be considered a shortcoming in a research paradigm, but it is essential in the treatment of complex human beings with complex disorders. This supportive context does not undermine the observation that the neurofeedback accelerates progress in treatment. After all, the same clinicians have lots of experience with service persons who don’t have the opportunity to do neurofeedback, or who pass on the opportunity.
When we survey the PTSD cases that have been uploaded to our symptom tracking data base by clinicians in a variety of settings around the world, some additional observations can be made. It appears that some one-fourth of trainees respond to the training quite rapidly, i.e. within ten to twenty sessions, and the improvement tends to cut across all symptom categories. About another half of trainees respond at a more typical rate, requiring some twenty to forty sessions for substantial symptom abatement. This leaves another quarter of trainees who either respond more slowly or, to judge by the numbers, not at all.
Brief Overview of Results
The results obtained at Camp Pendleton were recently presented in part at the 2011 Navy and Marine Corps Combat and Operational Stress Conference by three of the participating therapists, psychologists Michael Villanueva, Anna Benson, and Tamsen LaDou. Major Villanueva performed preliminary analysis on 350 cases for representative clinical categories. Each person’s training trajectory was fitted with a linear projection, irrespective of the number of sessions. An average regression line was determined from all of the individual projections, and an effect size was calculated. The most common complaints related to sleep quality, involving some 200 out of the 350. An effect size of 0.8 was obtained. Irritability was an issue with more than half of the participants (164), and yielded an effect size of 0.96. About one-third complained of being unmotivated (114), and that category yielded an effect size of 1.0. Slightly less than one third complained of depression symptoms (104), and yielded an effect size of 0.84. About one-fourth complained of migraines (83), and this category yielded an effect size of 0.5. The regression curves for depression and migraine are shown in Figures 1 and 2. (They are taken from the presentation at COSC. The material is available for viewing on-line at: http://cosc.sclivelearningcenter.com/index.aspx)
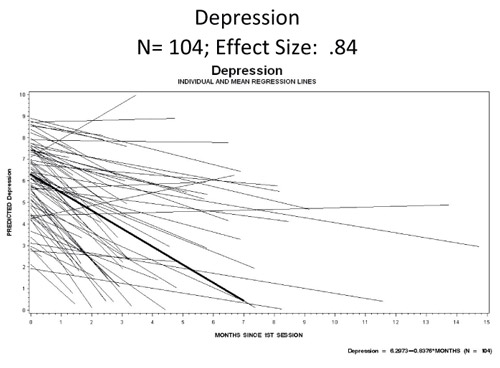
Figure 1
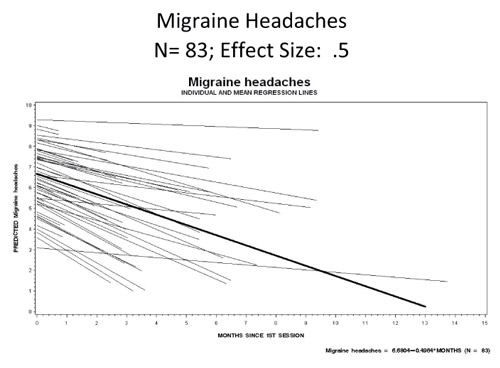
Figure 2
Effect size is not the best way to assess these data. That is because there is no pre-selection here on severity, as there would be in a formal research program. So the standard deviation is very large, and that goes directly into the effect size calculation. We are not just trying to demonstrate a clinically significant effect here. We are trying to solve the problem of depression in PTSD. So the tracking of symptom severity in the PTSD population is actually the more revealing. Such data (taken from our symptom tracking data base) are shown in Figure 3. This chart shows symptom trends for 81% of the population being tracked for depression. 19% were placed in the bin of slow- or non-responders, data for which are not shown. The different lines show data for those who spent different lengths of time in training.
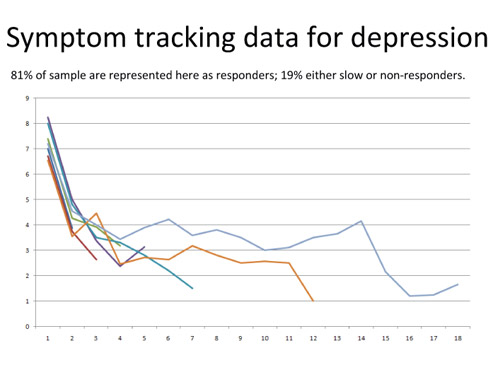
Figure 3
This plot shows that substantial relief from depressive symptoms is obtained by four out of five of the participants. The initial quick response across the board is quite striking. This uniformity of behavior argues for a common underlying mechanism, one that is clearly accessible to us in EEG feedback. Anyone familiar with pharmacology for depression will recognize that no drug known to man comes close to such results as are shown here. So two conclusions are apparent: 1) Depression lies largely in the functional domain, and 2) Remediating depression in PTSD is not contingent on resolving some presumptive chemical deficiency. Since these results exceed what can be achieved with anti-depressant medication, the need for placebo-controlled studies of this method is obviated.
Results of this kind have been obtained for all of the classic symptoms of PTSD. Strictly speaking, however, the target of neurofeedback is not PTSD per se, but rather physiological disregulation in general. So in order to ascertain how well neurofeedback effects remediation, one should look broadly at all symptoms of disregulation, as already suggested above. When the net is cast that broadly, case data accumulates eventually even for symptoms that are relatively rare in the population (i.e., incidence at the level of 1-2%). Thus it is found that all cases of reported suicidality have responded to date. Even though the numbers are small in this case, this does accord with our prior clinical experience with suicidality. Similarly, nearly all cases for the following conditions have responded well to neurofeedback: hypertension, heart palpitations, irritable bowel, chronic constipation, and asthma.
If all these results are regarded in isolation one from another, then indeed there is insufficient weight to be attached to any of them to draw significant conclusions. If, on the other hand, they are seen as different aspects of the same argument, namely that each of them is a signature of disregulation, then collectively they present a stronger case that indeed neurofeedback is resolving the physiological disregulation secondary to PTSD.
The Targeting of Physiological Disregulation in PTSD
The essential departure from conventional therapies lies in the direct targeting of physiological disregulation that is the basis of EEG neurofeedback. It has this feature in common with all of biofeedback. Indeed, evidence has already been brought to bear that a combination of various biofeedback techniques can be used for the remediation of PTSD. This ground has been covered well in a recent publication by psychologist John Carmichael. (Reference)
What then sets EEG neurofeedback apart? On the theoretical side, most likely it is that we have more direct access to the behavior of our neuronal assemblies, which is where the disregulations of PTSD play out. The frequency-basis of the organization of the EEG allows EEG feedback to interact with the brain in its most critical regulatory task, namely the temporal orchestration of the entire neural network across the entire EEG spectrum in every moment. This kind of EEG training has traditionally been done in the mid-range of EEG frequencies, and this is still typical to this day. But this cannot be all. The real breakthrough in application to PTSD came with the development of Infra-Low Frequency Training, with what we now call the Othmer Method. By operating at very low EEG frequencies, in the range of what is called the Slow Cortical Potential, we are able to witness fluctuations in cortical excitability directly, and to impinge on them in feedback configuration.
Quite generally, the problems addressed in EEG feedback can be modeled in two dimensions: the up-down axis of activation and of neuronal excitability, on the one hand, and the lateral axes of functional connectivity of cortical networks, on the other. It appears on the face of it that much can be accomplished in the remediation of PTSD simply by moderating network excitability, and that functional connectivity must tend to normalize in consequence. The rapid response that is so commonly observed argues for a one-parameter model, namely that there is one principal factor that governs the quality of cerebral regulation. If indeed there is one factor, then the evidence from ILF training points to cortical excitability.
It is likely that the first consequence of targeting neuronal excitability with the infra-low frequency training is the moderation of central over-arousal, along with the amelioration of autonomic hyper-reactivity. This is then deemed to initiate a virtuous circle that in turn acts back upon the neural networks, by virtue of the unitary quality of our regulatory regime, resulting in improved functional connectivity across the full EEG Spectrum. The advantage of working in the infra-low frequency region may therefore lie in the direct access this yields to both central and autonomic arousal.
Now the seasoned biofeedback therapist may respond to this hypothesis by pointing out that traditional biofeedback has been covering this ground of autonomic regulation for a long time. The case for the apparent superiority of EEG feedback in application to PTSD, if any, must therefore bring additional arguments to bear. There is in fact a significant point of difference between the two in implementation. ILF EEG feedback turns out to be highly sensitive to the particulars of the reinforcement. It is strongly dependent on placement, first of all, and it is exceedingly sensitive to the particular reinforcement frequency that is selected. No comparable parametric sensitivity has ever been observed in biofeedback based on peripheral physiology.
The high parametric sensitivity of the ILF EEG training may be due to the fact that we are using bipolar placement exclusively. This means that we are not just training the up-down arousal axis but rather also the functional connectivity between the targeted regions. So with this single approach we are appealing to both dimensions of the regulatory challenge, that of activation and that of functional connectivity.
We interpret the incredible sensitivity in working with the ILF regime to mean that we are interacting with the brain’s resting state networks. Their organization in the frequency domain apparently extends down to the exceedingly low frequencies at which we are currently working most effectively. Our signal bandwidth now extends down to 0.1 mHz (milliHertz), and if the band edge is even moderately raised, the results are distinctly different. The strong response we observe in real time to reinforcement in these low frequency regions implies that the resting state networks are highly constrained, and that any ‘interference’ with their organization in the domain of timing and frequency is strongly resisted. This constraint is always going to be much greater in the domain of functional connectivity than in the domain of activation. Hence our dependence on bipolar placement.
Under the above circumstances, neurofeedback can be seen as a very subtle challenge to resting state network functional organization, and the repetition of such subtle challenges eventually brings about a more robust regulatory integrity for these networks. In view of the fact that all of observable brain function is contingent on the functional integrity of the resting state networks, it can easily be argued that by means of this ILF challenge we are able to affect the entire realm of cerebral regulation. The evidence for that should show up throughout the EEG spectrum.
Whereas the above is quite possibly the heart of the story, it is surely not the whole story. In most cases we have looked at, the one-parameter fit only goes so far, and beyond that point we observe increasing dispersion in recovery curves for different symptoms. This is unsurprising, and thus motivates the further maturation of the method. The surprise is just how far we can proceed in general symptom abatement with a method that is quite simple in concept and design, if not in actual execution. The surprise is the breadth of impact of EEG feedback across functional domains, the consistency of response across a disparate list of symptoms, and the oftentimes rapid pace of recovery. The same method that renormalizes autonomic response patterns also impinges favorably on emotional regulation, on sleep architecture, as well as on executive function, cognition, and memory. For these reasons, ILF EEG feedback can be used in a seamless strategy that begins with symptom abatement and ends with an optimal level of functioning of the individual. This is what justifies our designation of these findings as a breakthrough.
The Implied Model of PTSD
It is inevitable that one’s view of the clinical condition being targeted is strongly influenced by the means being used to address it. Thus the pharmacologist is inclined to take the perspective of disturbed neurochemistry. The psychologist will trace the core issues of PTSD trace back to the original cause in emotional trauma, and they are therefore to be seen mainly in psychological terms. And the neurofeedback clinician is likely to see PTSD in terms of disturbed or disrupted neurophysiological function, essentially a deficit in self-regulatory capacity. In the pragmatic tradition of the United States scientific enterprise, one might be guided in our views on this issue by what actually works in practice. If targeting neurophysiological disregulation can effectively resolve PTSD to the point of clinical insignificance, which now appears to be routinely possible, then does that not also go to the issue of the essence of PTSD?
Consider that nothing involved in this therapy ever deals with the content of the traumatic memory. Conversely, consider that dealing with the content of the traumatic memory (as, for example, through exposure therapies) does not systematically lead to the resolution of PTSD. The living traumatic memory may play only a minor role in sustaining the ongoing misery of the PTSD sufferer. We may instead regard the original threat to the organism, the original traumatic event (or succession of events), as having metastasized into the physiology broadly, where it then compounds its damage by affecting multiple regulatory systems. Disregulation, if left un-remediated, begets further disregulation.
We have the very clear evidence that the descent into full-blown PTSD is often mediated by a succession of traumatic events, each of which contributes its bit to the causal chain. Just what is it that connects these events in the causal chain? It is the lingering disregulation they provoke in cerebral control mechanisms, autonomic regulation, arousal regulation, emotional control, and so forth. We have corroborating evidence for this compounding of vulnerability from minor traumatic brain injury, the consequences of which are in many ways similar to what we see in PTSD. We call such a concatenation of disruptive events the disregulation cascade.
We also have the experience of the traumatic memory itself. Before a person undergoes neurofeedback, memory recall may trigger full-blown re-experiencing, involving the full physiological response that was evoked in the original event. After successful neurofeedback training such recall will be experienced benignly, without triggering a strong physiological response. This demonstrates that what PTSD sufferers find disturbing is the physiological response rather than the original memory alone.
All of the above justifies making physiological re-regulation the primary target for the remediation of PTSD, and one could even go so far as to say that the essence of PTSD lies in the physiological response rather than the precipitating trauma. The time for psychotherapeutic remedies is after the physiology has been reasonably stabilized, not before. And the occasion for pharmacological remedies arises only after brain training has shown itself inadequate to the task of functional re-normalization.
The Road Forward
Sufficient clinical and theoretical information already exists at this time to be assured that EEG feedback in the Infra-Low Frequency region constitutes a comprehensive remedy for the lingering consequences of PTSD. In the simplest terms, PTSD disrupts the functional organization of cerebral networks, and EEG feedback restores their functional integrity. More specifically, our resting state networks are foundational to cerebral network functionality generally, and EEG feedback in the Infra-Low Frequency region appears to access those networks most directly.
The clinical results being obtained lie outside of the range of prior experience. Hence there is little question that the new method is better than all known alternatives. Once this is recognized, this knowledge brings with it an ethical obligation: Every returning service person ought to be given the opportunity to train his or her brain to restore it to optimal functioning status. At some level, everyone exposed to combat pays a price. We are now in a position to pay them back in the best way possible—with a nervous system restored to optimal functioning.
In the real world, a baleful asymmetry is at work in which bad news travels fast, and good news travels slowly. We are aware that the ‘system’ of care for veterans is not easily nudged toward change. Good news is handicapped at every turn by the patron saints of the status quo. One wishes that this process could be somehow accelerated. This newsletter is intended, among other things, to serve as a call to action to the mental health community in general, and the Department of Veterans Affairs in particular, to implement this new approach in a comprehensive strategy for the re-integration of our veterans back into our productive society.
This newsletter is also a call to action to the military to implement this method not only in the recovery of active duty personnel impacted by combat stress, but to install it in boot camp for purposes of stress inoculation and optimum performance generally . An approach which is entirely based upon the enhancement of function lends itself well to broad adoption within the active duty military. Preparation for military service is all about fitness training. No great conceptual leap is required to add brain training to that regimen. No diagnostic thresholds need to be met to qualify. Literally everyone can potentially benefit from brain training, irrespective of their initial level of competence. In fact, the more competent the brain is at the outset, the more it can potentially benefit. So this method is not simply targeting dysfunction. Hence, it fits readily into the culture of optimum performance and the standards of personal fitness that reign within the military.
References
1. Carmichael, John, (2010). Multi-Component Treatment for Post-Traumatic Stress Disorder, An ISNR Publication






Very interesting data, Sigfried. I hope military treatment protocols are moving towards making neurofeedback available to all personnel.
It would be interesting to survey the slow responders to see if they had depression/PTSD before entering the military. If they did, it would help to explain their longer recovery time.
I found this the most thoughtful, instructive and helpful outline of the current direction of thinking with respect to ILF use in NFB that I have encountered. It provides a clear framework for thinking about or analyzing what it is that we are actually doing when we begin work using this approach. And the reason I find this so important is that – finally – it provides a way of seeing mental disturbances with their attendant emotional, behavioral, cognitive and physiological effects – of seeing all these in terms of one underlying and reachable process. It is like a light was turned on in a dark room, a page is turned, and a door opens to a qualitatively new understanding of reality.
Siegfried, Congratulations! This is another superb explanatory essay. You take off from impressive the Villaneuva data, and then examine a helpful model of the physiological dysregulation in PTSD. (And where is John Carmichael’s publication?) Your next section, the complex systemic model of PTSD is very well done (the causal chain involves lingering dysregulation that “…provoke(s) …cerebral control mechanisms, autonomic regulation, arousal regulation, emotional control, and so forth”). Your reminder that neurofeedback has positive effect far quicker than medication effects is an important message to psychiatrists.
Thomas M Brod MD, DFAPA
Associate Clinical Professor, Psychiatry
Geffen UCLA School of Medicine
Thank you, Dr. Brod, for your message.
The book by John Carmichael is titled “Multi-Component Treatment for Post-Traumatic Stress Disorder,” and is available through the ISNR. I did not have it handy at the deadline for the newsletter. We wanted to post it for Memorial Day. We are adding the book reference. It helps to make the case for applied psychophysiology in application to PTSD.
Rachelle:
My own suspicion with regard to the slow responders is that we may be dealing with another class of PTSD sufferers here. Our work is really geared toward dealing with shock trauma or event trauma, the classic PTSD picture that informs the DSM model of PTSD.
Increasingly it is recognized that we also have to deal with relationship trauma, involving the loss of a close companion or loved one, and with the trauma of moral hazard, where the service person gets involved in activities that transgress personal moral standards, and for which he is later unable to forgive himself.
In these cases, I believe that we probably need a lot more Alpha-Theta training, and the fast pace of military service does not allow for enough of that.
There is also the factor that is known to all mental health workers in the field, which is that people slated for disability payments don’t want to do anything that might threaten the cash flow, such as it is. We have seen this as well, with clients (civilian in this case) terminating neurofeedback for the reason that if they felt any better, they would not feel right about continuing to get their disability check! It happens.
Great post , now lets hope the military allows all personal to use it.
I have been reading about PTSD. I have a case where the client is afraid of treatment based upon his disability check. I do not think this client has PTSD, rather anxiety from current life relationship problems in his marriage. I base this as he has managed to function very well in his life and stay extremely active, until the start of his divorce and the decline in the housing industry which was his main source of income. The individual went from a productive, very active person to divorce, unemployment and disability based 40% on PTSD from the Gulf War. The patient went to five Psychologists before finding a nurse practitoner and Psychologist that both wrote a letter stating they agree with the patient’s evaluation of PTSD. All doctors before clearly state how upset the patient was when they refused to give him a PTSD disability letter. I also found out the patient was never in combat as his sole position was recreation facilitator at the pool. The patient staes he found out he was being followed and investigated for involvement with individuals outside of the US forces, he saw a car on fire and watched as a woman was being taken for punishment by stoning although he states he never actually saw anything, just heard about it. The indivdual is extremely active with extra curricular activities, is jovial and the center of attention at all times. A far cry from what he tries to portray to the doctors. I also found out he was filing for unemployment benefits and receiving them and making up fake employer interviews, while he was vacationing in Florida, got re-married and fighting a custody battle. How can anyone be given a diagnosis of PTSD without even going into an in-patient facility for evaluation? especially with all the extra distraction adding to his anxiety hence limiting his capacity to cope with life on daily basis both mentally and physically? we all know emotional exhaustion from anxiety and stress is hard if not harder to cope with than physical exhaustion. How does someone know if the person is a ‘ticking time bomb’ in need of help or if he is beyond help? they gave him a disability of 40%. It seems to me, he would benefit greatly from rehabilitation therapy.
Cases where symptoms may be faked are problematic indeed.
This is where our non-profit activity Homecoming for Veterans (www.hc4v.org) can play a unique role.
Since the neurofeedback service is provided to veterans at no cost under that program, this can clarify the issue of whether the person is actually interested in getting well.
If the offer is spurned, then one might question the claims with regard to the actual suffering being endured.
Siegfried Othmer
Ok