Remediation of PTSD using Infra-Low Frequency Neurofeedback Training
by Siegfried Othmer | March 7th, 2012 The careers of the scientist/practitioners in the field have undoubtedly had in common the experience of gradually rising expectations about what is possible to achieve in terms of improved self-regulatory capacity and mental functioning with the aid of neurofeedback. One might have expected some plateauing after a while, a firming up of one’s expectations, but the surprises keep coming and they are consistently on the upside. In our own experience, one of the biggest surprises has been the growing effectiveness of neurofeedback with PTSD, along with the related conditions of developmental trauma and the autism spectrum. All of these conditions had seemed so utterly intractable in the past.
The careers of the scientist/practitioners in the field have undoubtedly had in common the experience of gradually rising expectations about what is possible to achieve in terms of improved self-regulatory capacity and mental functioning with the aid of neurofeedback. One might have expected some plateauing after a while, a firming up of one’s expectations, but the surprises keep coming and they are consistently on the upside. In our own experience, one of the biggest surprises has been the growing effectiveness of neurofeedback with PTSD, along with the related conditions of developmental trauma and the autism spectrum. All of these conditions had seemed so utterly intractable in the past.
In this newsletter, the focus on PTSD exists not only for its own sake, but also to serve as the best vehicle for the tackling of larger themes. What sets PTSD apart from our clinical work in general is the concentrated effort that has gone into this area by virtue of the great need among our returning veterans. We have attempted to meet this need through a non-profit entity, Homecoming for Veterans (hc4v.org), which has attracted even international participation among clinicians. As a result of these collective efforts, a large database of clinical results has been gathered that is now available for “data-mining.”
This collection of data has allowed us to firm up some expectations even for those PTSD symptoms that are not commonly encountered in an individual practice. The data have the significant advantage of being drawn from a wide variety of sources, and therefore include contributions to outcome variance that would not be an issue in a formal research design. This gives any findings an intrinsic robustness that could not be matched in any single funded study. The accumulated data are relevant to clinical effectiveness in realistic settings, and thus answer the probative question that confronts policy-makers.
Infra-Low Frequency Training
The training technique used almost exclusively in this work is the Infra-Low Frequency (ILF) training that we have developed over the past six years. The training can still be considered in the same frame as traditional frequency-based neurofeedback, in the sense that the training effects are highly frequency-specific. But in this low frequency range, where a full cycle can take over an hour, the standard signal-processing techniques are not applicable. One has no choice but to abandon that approach and move simply to signal-following, or waveform-following, by analogy to what is commonly done in peripheral biofeedback. The neurofeedback trainee just observes the evolving time course of the differentially amplified slow cortical potential. There is no threshold, and there are no discrete rewards. The process is no longer one of operant conditioning as generally understood.
In the case of infra-low frequency training, the differentially-derived signal undulates between positive and negative phases, and one is not more virtuous than the other in the process of the brain engaging with the signal. Standard reinforcement procedures lose their meaning in this context. The brain interprets the signal in terms of its own internal activities through a continuous process of correlation. As the brain recognizes its relationship with the displayed signal, it attempts to project that signal forward and bring it under its own overt control. None of the elements of this process are free of error, and therein lies the basis for a perpetual challenge in which the brain attempts to reach closure between its internal state and the interpretation it assigns to the slowly migrating signal. The brain will have internalized the control loop and made it the functional equivalent of the other internal control loops that are involved with issues of state regulation.
A PTSD Case Report
With this brief description of the process, we turn to an actual case report. The training history of a veteran with PTSD is illustrated in Figure 1, where symptom-tracking data are shown for the dominant complaints. This case was chosen over others for two reasons. First, this individual had a larger than usual list of significant complaints, and secondly the training was done in our own office, so we have familiarity with this person beyond the data. In this case as in all others, a wide-ranging initial clinical interview established the critical issues for this person. These are quantified here in terms of severity on a Likert scale of 0-10. (The initial symptom list included several hundred items, of which some 60 are commonly reported in PTSD. Twenty-five of the more significant symptoms in this case are shown in the illustration)
Figure 1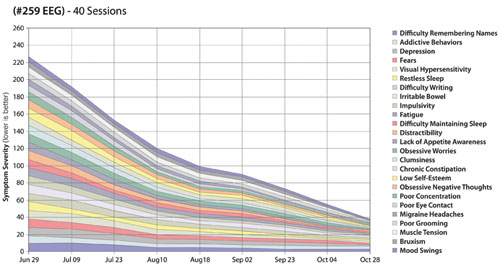
The impression given by the results of brain training over time is one of joint resolution across the seemingly disparate symptom categories. The similarity in learning curves is more clearly reflected in Figure 2, which just replots the same data. It is noteworthy that this list includes such varied symptoms as depression, bruxism, migraine, irritable bowel, addictive behaviors, and chronic constipation. All of the symptoms move toward clinical insignificance at a similar rate over the period of forty training sessions. This pattern is a common observation within the entire data set of nearly 400 cases.
Figure 2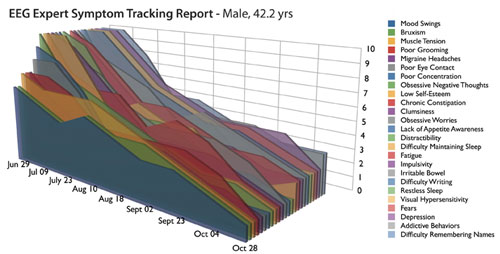
PTSD in the Disregulation Model
This striking commonality in learning curves across the board allows us to reframe the issue of PTSD as a disorder of disregulation. Resolve the disregulation and the symptoms collectively diminish to clinical insignificance. If this kind of reframing is supported by the collective data set, then it is appropriate to shift attention to the disregulation status per se, and attempt to resolve that by whatever means are at our disposal using primarily the methods of applied psychophysiology. With the adoption of this perspective, all symptoms of disregulation become criteria by which we judge our success in restoring self-regulatory integrity, quite irrespective of whether or not these are regarded as classic or defining symptoms of PTSD.
Regarding PTSD as primarily a psychological condition has been an understandable but unfortunate misdirection. This is not to say that traditional psychological approaches are entirely irrelevant to the resolution of PTSD. Rather, it is to argue that these play a supportive role, particularly in the early phases of recovery. Much of the success of exposure therapies is also traceable to physiological normalization, an objective which can now be achieved much more readily and with less drama with psychophysiological techniques. Once the physiology has been stabilized, there is much to be done with psychotherapeutic methods. But by that time PTSD will likely no longer be diagnosable.
Overview of Symptom Tracking Data
So what do the collective data indicate with respect to the recovery of regulatory integrity using ILF feedback? In broad brush, trainees can be grouped into three principal groups: 1) A rapidly responding group consisted of nominally 25% of the population. Here functional recovery could be achieved within twenty sessions, with a median value of less than 10 sessions. 2) A conventionally responding group in which recovery was achieved within 20-40 sessions, in line with common expectations within the field for a variety of indications. And 3) a treatment-resistant group in which recovery could not be achieved by the time training was terminated. This group consisted of nominally 25% of the population.
These divisions are reflected in the trends seen with the most common symptoms. Thus flashbacks of trauma were found to resolve in 75% of the trainees. Panic attacks largely subsided in 80%. Agitation responded in 70%; likewise irritability; anger resolved in three out of four. Anxiety and depression responded very similarly, becoming clinically insignificant in about 80% of cases. Fears resolved in two-thirds of cases. Sleep disregulations responded in a manner representative of the entire data set, with nominally 25% rapid responders and some 50% typical responders. One exception was night sweats, where there was 80% favorable response and nearly half of all cases responded rapidly. The most favorable outcome was seen for migraines, where less than 10% were either non-responders or very slow responders, and some 40% of cases were in the rapid-response category. Muscle tension headaches, by contrast, were found to respond in 75% of cases.
The most intractable symptoms were tinnitus, where only 50% were observed to largely resolve their symptoms; chronic nerve pain (40% response); and joint pain, where the recovery was only partial, and observed in less than 50% of cases. On the other hand, all cases of stomach pain responded, as did all cases of jaw pain, of hypertension, of chronic constipation, of asthma, and of skin rashes. Heart palpitations responded in 80% of cases; irritable bowel resolved in 80%; and allergic sensitivities eased in 80%. Overall more than 200 symptom categories were evaluated in this survey, of which some 60 were prevalent in this population.
Training Protocols
All of the training was accomplished with essentially four electrode placements: right parietal training for physical calming; right frontal training for emotional calming and control; inter-hemispheric training for brain stability; and left frontal training for recovery of executive function. Either T3 or T4 was common to all placements. If one surveys the whole population, the modal value for the number of sessions to reach effective resolution was less than ten, which means that the greatest likelihood was for rapid remediation of symptoms. In such a small number of sessions probably only a single protocol was utilized, or perhaps two.
This observation helps to consolidate the case for the disregulation model of PTSD. It is the same two protocols, after all, which are the starting points for all of our clients, irrespective of diagnosis, and this is all being done within the frame of the disregulation model. Either there is a rather simple core deficit underlying all of the disparate symptoms being addressed in PTSD, or the simple challenge which the brain undergoes in ILF training manages to reorganize the whole system despite its complexity. Or both.
Historical Development of ILF Training
Before we take this further, one must also ask whether the quality and comprehensiveness of the above results collectively are attributable specifically to the ILF training. It is unquestionably our clinical impression that the ILF training has allowed us to do our best work. But we can also bring some supportive evidence to bear. The story goes as follows: We have been individualizing our training for well over a decade now, and have observed a gradual trend to lower and lower reward frequencies over the years, with the further development of clinical expertise. The modal value in the distribution of reward frequencies tended always to be the lowest frequency we had available in software. For years this was limited to 1.5 Hz because the software utilized 3-Hz bandwidth.
The extension of the target frequency range down to 0.05 Hz occurred in June of 2006, and it was in this step that the transition to waveform-following became necessary. During the initial six months of getting acquainted with the new approach to feedback, some 52% of clients optimized their training at the lowest frequency. Over the subsequent six months, this dominance increased further to 66% as more familiarity was gained with the low-frequency techniques. More than 250 clients were involved during this phase. With the extension of the target frequency range to 0.01 Hz in 2008, the same pattern was observed: 65% trained optimally at the lowest available frequency. With the further extension to 0.001 Hz soon thereafter, the percentage training at the lowest frequency rose to 77% over a period of time as clinical skills were honed. The range was further extended to 0.1 mHz (0.0001 Hz) in March of 2010, and over time more than 85% of patients ended up at the lowest target frequency within their first few sessions. With the accumulation of additional experience, as well as more data for better statistics, this percentage reached 90. It appeared that the lowest target frequency was the best tolerated as well as the most effective. Notably, with each extension of the range to a lower limit, the clinical reach extended to more complex clinical presentations that had not responded well earlier, and outcomes systematically improved.
The trend in target frequency distribution is certainly paradoxical for a number of reasons. The more we extend the target frequency to lower limits, the more the client population congregates at the lowest value. The opposite was expected. One would have thought that at some point the population would distribute itself more broadly across the newly available spectrum. Of course this is not what is happening. As the target frequency is extended downward to lower values, the information at higher frequencies is correspondingly attenuated. It is not that more information is being made available at the lower frequencies with the downward migration of the target frequency, but rather that less is being made visible at the higher frequencies. This means that the brain is essentially being compelled to pay attention to the lower-frequency constituents of the signal because there are no distractions from information at the higher frequencies. Obviously the brain is going to pay preferential attention to the more dynamic higher-frequency constituents of the signal, so the only way to force the brain’s attentions onto the more languid, slower components is to blind it to the faster components.
As the target frequency is lowered, therefore, the principal change is one of a reduction in the effective signal bandwidth. A second paradox, then, is that the lower we set the target frequency, the less information is being presented back to the brain per unit time, and yet clinical outcomes are not only better, but are achieved more rapidly as well as more consistently. The clear implication is that the lowest-frequency constituents of the signal are the most salient, despite the fact that they afford the least amount of information on the prevailing EEG dynamics. This is a direct challenge to our usual understandings of how feedback loops behave, and it must have a non-trivial explanation.
The Training of Resting State Functional Connectivity
All of the above makes sense if we postulate that the ILF training is efficiently re-normalizing the functional connectivity of our resting state networks, and that the relevant information to achieve this most efficiently lies at these very low frequencies. EEG feedback has largely been about the training of resting states of the system. SMR training was first modeled as a calming of motoric excitability. Alpha training is certainly about training the brain toward calmer states as well. Biofeedback techniques are oriented toward calming autonomic nervous system over-activation. It is in the nature of our resting states that they persist over time, and to the extent that they are functional, they will resist ‘outside’ interference. By operating at these very low frequencies, we are challenging resting state functional organization where it is most persistent, and intrinsically most resistant to interference. Hence an even subtle challenge can evoke a response by the brain, which over time and with repetition mobilizes its functional re-organization.
Let us take a more ‘wide-angle’ perspective on all of the above. The facts before us are that all of the symptoms of disregulation that makes their appearance within the penumbra of PTSD resolve to a greater or lesser degree with a very simple protocol, or small set of protocols, acting upon the functional connectivity of our persistent states, which we now know to be organized around a modest number of resting state networks. There is no bias in this intervention; no directed challenge; no explicit targeting. The brain is simply responding to information about itself, about its own instantaneous state. The immediate impact is on activation and tonic arousal, with a longer-term impact on the regulatory ambient of arousal and of specific network activations.
This in turn implies that the myriad symptoms we tracked can be seen as grounded in the disregulation of core regulatory functions—of central arousal, autonomic balance, affect regulation, vigilance, executive function, and of motoric excitability. The results indicate that improving state regulation is sufficient to render most of these symptoms clinically insignificant. This feature of neurofeedback, namely that we obtain broader benefits from the training than we feel entitled to for our modest efforts, has been noted even from the early days of SMR and alpha band training. It is also characteristic of peripheral biofeedback.
In fact, the method of ILF training bears more resemblance to traditional biofeedback than to conventional frequency-based neurofeedback. It bears the greatest resemblance to heart rate variability training, which also happens to be the most promising approach to PTSD among the biofeedback options. It seems appropriate at this juncture to try to find common ground in the mechanistic underpinnings of our respective tools.
It’s Relaxation Training After All
We may finally be in a position to give a more scientific description to what we have been calling relaxation training. Our brains’ functionality rests ultimately on the functional integrity of our resting state networks. But how does one access these? Unburdening the system by quieting body and mind takes us there by a variety of means; increasing the amplitude of our cortical resting frequencies can take us there; and perhaps the witnessing of our own resting state network activity takes us there most efficiently. We can finally tell the FDA forthrightly that what we are doing is relaxation training after all. That claim was starting to look a bit threadbare.
Feldenkrais was perhaps the first to appreciate the advantage of working near the least-challenged state, the still-point of the motor system, in order to improve its regulatory capacity. ILF feedback can likewise be seen as still-point training across all of the relevant regulatory domains concurrently. Its therapeutic complement is Alpha-Theta training, the other key contributor to the resolution of PTSD. This can also be understood as a kind of still-point training, a quieting in the psychological domain. At the time of Eugene Peniston’s work, the emphasis was largely on the alpha training component of the Menninger protocol. With the emergence of ILF feedback, Alpha-Theta training has been eased into more of a supporting role, and sometimes a minor one at that. This is testimony to the fact that as our effectiveness in regulating our physiology grows, the burden on heavy-duty psychological interventions is reduced.
PTSD in this model can be described most simply as a disruption of resting state network functional connectivity. The cerebral turmoil of a severe emotional trauma, or of a concatenation of minor traumas, bars a return to quiescent baseline states in some people. The same holds true in minor traumatic brain injury, with physical insult added to the emotional impact that surely must also accompany TBI. And a similar mechanism is operative in schizophrenia, in the autistic spectrum, in developmental trauma, in addiction, in the dementias, and in chronic pain syndromes.
In all of these cases, the first resort should be to retrain the brain toward integrity in resting state functional connectivity. Over time, we benefit from a virtuous cycle in which control systems regulate each other as opposed to disregulating each other. At some point of course the incremental benefits diminish, and if necessary one adds on other methods—many already well-established within the field—to complement the ILF training. So we are not claiming that ILF training is the ‘universal solvent’ of the neurofeedback world. But it does appear to get at the core of the most intractable psychopathologies, and is therefore to be recommended as the central focus, and in particular as a starting point, of neurofeedback strategies in the general case.
Finally, a note of caution must be sounded. What is probably a general rule in feedback applies to ILF training as well: The stronger techniques place the greater burden on the clinician for proper direction and management of complex clinical presentations. Readers may be enticed by the above to rush into practice with ILF training simply because their instrument allows it. That temptation should be resisted until proper training has been undertaken.
Conclusion
In conclusion, the evolution of Infra-Low Frequency training over the last six years has given us a technique that bridges the disciplines of traditional biofeedback and of conventional neurofeedback. It is frequency-based in its construction, along with the rest of neurofeedback, and yet one is training on a time-domain waveform that is more characteristic of biofeedback. This waveform tracks the transitions in differential activation in real time, as seen through the shaping function of the operative ILF band-pass filters. ILF training is an alternative to biofeedback for restoring autonomic regulation, and it exceeds prior neurofeedback approaches to affect regulation. These are the principal keys to the resolution of PTSD, which ILF training accomplishes efficiently.
All this is best understood in a systems perspective in which core regulatory functions are targeted as a first priority, yielding comprehensive coverage of the state regulation issues that dominate in psychopathology. Of course ILF training is not exhaustive, either in the perspective of neurofeedback or of biofeedback. In application to complex disorders such as PTSD, and with the objective of optimal functioning in mind, multiple brain challenges are called for. That means bringing our “multiple intelligences” to bear from a variety of scientific and clinical perspectives. It is time to break down the internal barriers within our discipline to bring that about.






Very interesting work and results…thank you for your contribution to the understanding and common resolution of myriad issues! Curious about your understanding of the treatment resistant group. What do you see as common attributes of that population? Is it currently possible to predict or screen that group prior to training? What other alternatives exist? Thank you. Patrick
We have obviously thought about this question at great length ourselves, and we have not been able to identify any one dominant factor that could explain the observed failure rate. Of course it should be noted that I have lumped the slow responders in with the ‘true’ non-responders. For the slow responders neurofeedback is still the best option, although the training will be a longer journey for them. It has been estimated that the ‘true’ failure rate would be around 5% if the training were to take place under more ideal conditions—regular sessions undertaken with sufficient frequency, and working with a seasoned clinician. I can also say that the success rate is improving over time, which can be attributed to better software and more refined training protocols along with more clinicians being further up the learning curve. These cases are complex, and they call upon a great deal of clinical skill, even though the basic technique is straight-forward.
One factor that is clearly in play is the concern among many that even with successful training they may end up in a kind of middle ground where they no longer qualify for disability support but are not yet in a sufficiently functional state for employers to want to hire them. As long as that uncertainty exists, the safer path may be not to acknowledge the progress that is taking place. A similar issue is commonplace in Workmen’s Comp.
We have considered an additional hypothesis, namely that many returning service members and veterans are struggling with what is called ‘moral injury,’ where they were involved in acts that deeply violated their own moral code. Or they may have suffered ‘relationship trauma,’ in which someone very close to them was lost in combat. Here we may be dealing with a deeper trauma than many others that may be less directly personal. It is possible that this ongoing turmoil works against us in trying to calm the physiological agitation.
Here we come up against a paradox in our work, in that while we do well with the abatement of the physiological symptoms of PTSD, we are at the same time also enhancing the capacity for empathy and for relationship. So in the event of moral injury or relationship trauma, the trainee may end up feeling these even more keenly than before. There is no possibility of erasure here—but we shouldn’t be asking for that in any event. This is our human condition. This is where support from the therapist and others comes in. We can even talk in terms of a network model for healing at this level, but this now involves an inter-personal network, and perhaps even a trans-personal one. These traumas cannot be expunged; rather, they must be incorporated into the self. In the general case, this cannot be done merely with boot-strapping our internal resources. It is accomplished in relationship and through connection with other healing resources.
Knowing all of this, our own moral burden is to make it possible for all of our returning veterans to have access to these resources. See http://www.homecomingforveterans.org
The increased awareness of feelings surrounding the trauma event(s) is the realm of synergistic techniques like EMDR or EFT. They work very well with NF in my experience. – JW
These methods are indeed complementary, but I am wondering if in your work with NF you are getting much opportunity to do Alpha-Theta training. I’d like to get more of a sense of how EFT and EMDR fit in with the Alpha-Theta training component. For example, do you hold off with EFT and/or EMDR until the time when you introduce the Alpha-Theta training? Do you then use one to potentiate the other? Or do you already bring these techniques into the picture while you are still doing the Infra-Low Frequency training?
After attending the Third Integrative Medicine for Mental Health Conference in Santa Fe this past summer, I wonder whether the treatment-resistant soldiers in the various studies had biomedical issues that trumped the effect of the Neurofeedback. In my own practice I have now seen several “failures to respond” that after some lab tests turned out to have some significant medical condition in their lower gut. One had candida albicans, another an overgrowth of clostridium dificile, and a third had systemic contamination by stachybotris black mold. Each of these conditions can adversely affect brain functioning in episodic and seemingly random fashion.
Thus my new axiom is to get a thorough medical history, probing specifically for any abdominal problems. Second, if I do not see any reduction in symptom severity, I push for blood and urine testing for evidence of metabolites of a number biomedical conditions, which might nullify the effect of the Neurofeedback.
I found this article on your website and find it encouraging however I see that it is dated 2012. Do you have any more recent findings to share? Thank you very much.
The method has been further developed since 2012, so that presently it is both easier to use and even more rapidly effective. It is being inserted into clinical practice in application to PTSD–and even to victims of torture–in many countries. We have just received a study done in Sweden under the auspices of the Red Cross there. The method was employed with refugees from the Middle East wars who were found to be treatment-resistant to conventional therapies. A number of them had been victims of torture. Their recovery was profound even in the span of twenty sessions. Gains were modest in the first ten sessions, quite possibly because the clinicians (who were new at this) needed to find their way with each person. Gains were then substantial in the subsequent ten session, although ideally one would wish for more sessions.
I forgot to mention that Carol Kelson performed a controlled study of ILF neurofeedback in application to PTSD for her Ph.D. dissertation in 2013. The subject population consisted of Vietnam era veterans living at the Bell Shelter of the Salvation Army in Southern California. These veterans had obviously been living with PTSD for more than forty years, and their functional deterioration was well advanced. The results were so positive that this study then grew into a full-bore adoption of ILF training into the range of services being offered to veterans at Bell Shelter. This has resulted in ILF training now being offered at three other sites within the Los Angeles area.
[…] A 2012 study suggests that neurofeedback involving very low frequencies—between 0.02 and 0.2 Hz—results in rapid significant reductions in the severity of PTSD symptoms. […]