
The subtitle of Thibault and Raz’s latest diatribe against EEG neurofeedback sounds vaguely promising: “Clinical Intervention even if Placebo.” But the ambivalence implicit in the title runs through the entire article. The tone of the paper is argumentative throughout, shoring up an essential posture of skepticism with respect to EEG-NF while also allowing for the possibility that we may have been right all along: there is something to neurofeedback after all. We appear to be witnessing the last stages of resistance by these neurofeedback deniers. A subtle repositioning is going on.
Whereas it is irritating to neurofeedback practitioners to have to come to terms with yet another assault on our understanding, our competence, and even our integrity after all these years, the paper documents the abiding reality that academia has not contributed to the development of EEG-nf for over thirty years. Rather, academics have by and large conducted a sniping and hazing operation against neurofeedback from their fortified redoubt. They have resisted–or haughtily dismissed–promising developments at every turn. Progress in neurofeedback has therefore defaulted almost entirely to the clinical realm. Even the few academic studies that have come to our attention recently are pathetically naïve in their design and ham-fisted in their execution. Some of them smell of a death wish for neurofeedback.
Once again, Thibault and Raz hold the placebo model over our heads, faulting us for not taking it seriously. But the error is entirely theirs, not ours. The placebo model is relevant to neurofeedback in only a very limited sense: If the placebo is to prevail as the explanatory model of neurofeedback, then it must explain everything. If things happen in neurofeedback that cannot be explained in terms of placebo factors, then attention must necessarily shift to the new phenomenology, and the placebo model loses its privileged place in the discourse. At one point in the paper, the authors appear to acknowledge that their placebo postulate cannot explain all of neurofeedback: “EEG-nf works, but it likely relies heavily on placebo phenomena.” Hurrah! The essential divide appears to have been crossed even with some of the most stalwart holdouts. Now we can move the discussion to more fertile ground.
We hasten to stipulate that placebo factors matter in all of neurofeedback, but that is not a flaw. Both placebo (all placebo factors taken collectively) and neurofeedback promote the self-regulatory response of the nervous system, each in its own way. Both are feeding at the same trough, the abundant resource of latent brain plasticity. Whatever happens randomly under the rubric of the placebo can be achieved systematically with neurofeedback. In practice, the more placebo factors in the mix, the better. As has been said even forty years ago by Shellenberger and Green, the placebo is a compound of biofeedback, not a confound. If neurofeedback is not entirely reducible to the so-called placebo, then the word need no longer pass our lips. It is a mere grace note in the performance. It is an abiding presence in our work without special invitation. It takes care of itself, and need concern us no further. We are done here.
Thibault and Raz point out, correctly, that “If EEG-nf were a powerful and focal tool to modulate brain function in relation to specific behaviors, we would expect to see adverse reactions in some participants….” But we do! We do! Almost anything we can make better we can also make worse. It is adverse effects that have goaded the field toward refinement of its procedures over the last few decades. Adverse effects have even made it into the literature, driven by the adversarial realities that exist within the field.
But Thibault and Raz still manage to complain that “reports of negative effects remain anecdotal.” Just what do they expect? Of course these reports are anecdotal, just as is the case for Adverse Event Reporting in the medical field. If adverse events were systematic, the protocol would fall out of favor. Indeed, several protocol schemata have disappeared out of inventory for precisely such reasons. They were too plagued with adverse outcomes that could not be readily predicted or ameliorated.
Thibault and Raz cite one of our publications, and therein adverse outcomes are on full and forthright display. In a figure from the paper, participants are rank-ordered in terms of their pre-training impulsivity scores. The lines going down indicate declining scores with the first twenty sessions of training. Not all these adverse responses (those outside of test-retest uncertainty) can be blamed on neurofeedback, but many clearly can. In the case of adverse responses in the early phases, the training is typically continued with a different protocol. These data refer to the protocols used in the late nineties.
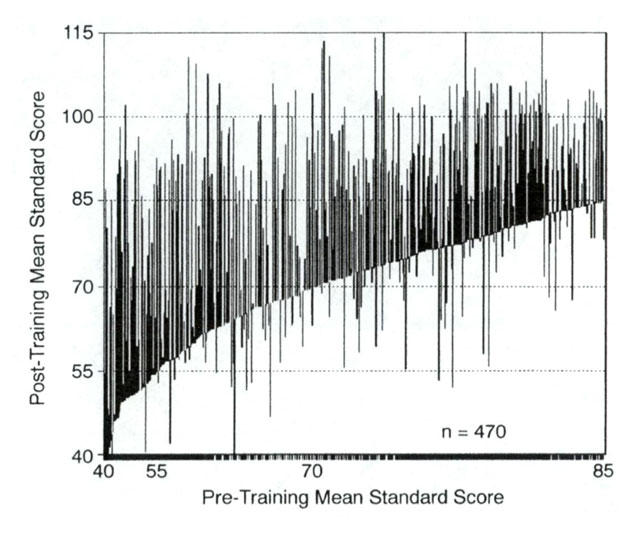
The above data are now nearly twenty years old. Matters have advanced considerably since then. It is clear by now that good self-regulation does not need to be purchased at the cost of side effects. These are not unexpected as clinicians find their way with highly dysregulated nervous systems. But they shouldn’t still be there when training goals are finally met.
Consider now the problem of adverse responses at another level. Thibault and Raz have felt entitled to inflict their views again and again upon their academic colleagues while apparently being quite ignorant of the fact that adverse responses have been a core concern within the field since its beginnings. Adverse responses have been the batakas with which contending schools of thought have been beating each other about the head since time immemorial. This demonstrates just how little they know about our field. They are self-trapped in their intellectual bubble.
Thibault and Raz dispute the argument that insufficient funding has gone into the field to permit the kind of fundamentally sound research that they call for. In support of their rebuttal, they cite—among others—our paper in which results on over 1000 cases were reported (Kaiser and Othmer, 2000). But that study was self-funded, so it goes against their argument. Our paper reported on a naturalistic outcome study from 32 private practices. It was not a research design. The intent was to educate ourselves on what was achievable in realistic settings, and then to share that with the community of professionals.
Their implicit indictment goes entirely the other way. Academia has defaulted on its obligation to study neurofeedback, and it has likely done so for a variety of reasons. These include a profound conceptual blindness at the theoretical level, as well as a visceral distaste for taking clinical work seriously at the sociological level. Additionally, we know that the pharmaceutical industry holds both academia and the funding agencies in intellectual captivity. On the one hand, academics call for the kind of large-scale RCTs (Randomly Controlled Trials) that are customary in drug trials, but then they refuse even to propose them, to get them funded, and to do them. They are plainly not interested.
In the final analysis, it must also be acknowledged that the field of neurofeedback does present a juicy target for the critics. As might be expected for a new scientific frontier, we have collectively made all the mistakes along the way. We have been handicapped by our own conceptual blinders at every turn. Just as the placebo cannot explain all of neurofeedback, neither can the operant conditioning model. To continue to insist that it does is just as delusional as the placebo as the exclusionary model of NF.
The Balkanization of the field; the protocol sectarianism; the proclamation of verities beyond the reach of evidence; the posturing and chest-beating that goes on; the rush to judgment; all this testifies to the fact that within our field we are just as subject to human foibles as the rest of the healthcare field. Problem is, as clinicians we sit outside of the tent. Behavior that is tolerated within the tent becomes a target outside of it.
What keeps us all going is the realization that we have found our way to a potential revolution in health care. This portends major impacts on early child development in particular, with potential payoff throughout the lifespan. There has not been a greater blunder in the annals of psychology, psychiatry and neurology in the last half century than ignoring the implications of the robust self-recovery capacity of the nervous system, and the role of the neuromodulation technologies in accessing and potentiating that capacity.
Clinicians are not scientists, and they are not statisticians, by and large. But they are stamp collectors–accumulators of invaluable clinical experience. What we possess in great abundance, and what our critics lack entirely, is clinical experience. What we know to a certainty is vastly in excess of what we can readily prove—particularly to the closed mind that does not wish to be persuaded. For our part, we decided long ago that engaging the critics is a fool’s errand. It is also completely unnecessary. That is not how a paradigm-breaking field advances.
What the desiccated and tendentious piece by Thibault and Raz misses is the human dimension of the process by which we all got here. None of us were born with the mission statement to promote neurofeedback. At some point a compelling event changed the direction of our lives. Sterman was a productive and successful animal physiologist until he was approached by Wanda Wyrwicka, his staff scientist, who told him insistently about his new discovery: “Barry, this is too important. You need to do this with people.” He did, and his career suffered in consequence because of the resolute obtuseness of his colleagues. Once in the grip of neurofeedback, he could not let go. The same was true of Joel Lubar, who persisted with neurofeedback very much against the grain of trends in his profession. Lester Fehmi abandoned a promising academic career at Stony Brook when he could not get funded for his alpha training research. Elmer Green found safe harbor at the Menninger Foundation.
When Sue and I experienced neurofeedback through our son Brian—and then on ourselves—we likewise could not walk away. For me, a physicist with a lifetime involvement with signal processing, and for Sue, a neuroscientist whose academic career had been aborted by our son’s neurological problems, this was not only the opportunity of a lifetime, but a keenly felt moral obligation. Our engineer friend and colleague Edward Dillingham committed three years to the development of software for our NeuroCybernetics system without pay—largely based on having seen the results with our son Brian.
By now well over a million people have benefited from our protocols; some 500 or more clients graduate from our kind of neurofeedback training every week. Nearly all of them had the experience of unsatisfactory outcomes from standard care before coming to neurofeedback. If they weren’t benefiting more than from anything they had done before, they would not have hung around for twenty sessions, not to mention forty, sixty, or more.
Hundreds of women are recovering from their war-related traumas in the Congo by means of our kind of neurofeedback. Thousands of service members have benefited from our methods for recovery from psychological and physical traumas at our military bases. Hundreds of veterans have received free neurofeedback services at Salvation Army shelters. Hundreds of clinicians offer neurofeedback at no charge to veterans through our Homecoming for Veterans program. Our methods are presently used for the recovery of torture victims—the most challenging of patients—in treatment centers of four European countries.
The field is much larger than critics realize. Collectively we have built a robust and technically competent enterprise. By now all the money that has gone into the development of neurofeedback instrumentation over the years is likely comparable to the total budget that President Obama allotted to his brain initiative: $100M. Only a minuscule portion of this was funded by the government, and very little was investor-funded. Most of the funding was supplied by the end user coming for neurofeedback services. This has been a boot-strapping operation in the best sense of the term. This has also been exploratory science at its best.
“The dawn of brilliant epochs is shadowed by massive obscurantism…rooted in human nature…the refusal to speculate freely on the limitations of traditional methods…The rejection of any source of evidence is always treason to that ultimate rationalism which urges forward science and philosophy alike.” Alfred North Whitehead
“He who studies medicine without books sails an uncharted sea, but he who studies medicine without patients does not go to sea at all.” – William Osler
Siegfried Othmer, Ph.D.
———–
References:
The psychology of neurofeedback: Clinical intervention even if applied placebo,
Robert T. Thibault and Amir Raz, American Psychologist, 72(7), 2017 DOI: 10.1037/amp0000118
Effect of Neurofeedback on Variables of Attention in a Large Multi-Center Trial,
David A. Kaiser and Siegfried Othmer, Journal of Neurotherapy, 4(1), (2000), pp.5-15
I’m glad to see Elmer Green mentioned here. He died in March at the age of 99. If it hadn’t been for Elmer & Alyce Green’s ‘Beyond Biofeedback’, I might never have heard of biofeedback and neurofeedback.