An Open Letter to Mark A. Reger, Department of Veterans Affairs
by Mark A. Reger | August 4th, 2025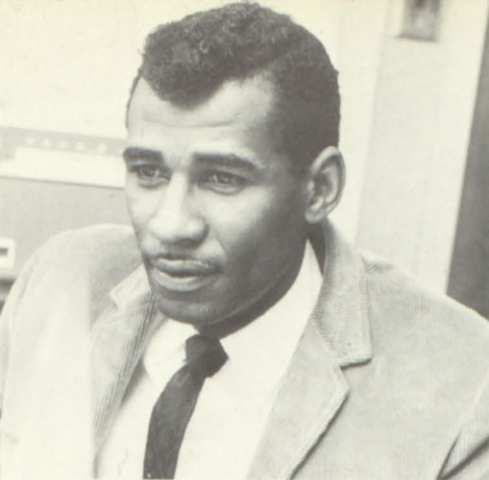
Eugene Peniston
Dear Dr. Reger:
I just read your article in JAMA with great interest. I would like to draw your attention to a recent publication on a controlled study of neuromodulation in application to treatment-resistant PTSD that was completed recently at the VA Pacific Islands Health Care System in Honolulu. It recruited 87 participants. This was a study of Endogenous Neuromodulation, a second-generation neurofeedback in which the brain is simply engaging with its real-time dynamics in the EEG and Infra-Low Frequency domains. This method has its roots in the early EEG neurofeedback, and thus has been under development for nearly forty years.
The paper, a pre-proof version, may be found here:
Dr. Judy Carlson, Dr. G. Webster Ross, Dr. Caitlin Tyrrell, Dr. Belkys Fiame, Dr. Courtnee Nunokawa, Dr. Chathura Siriwardhana, Ms. Kim Schaper, Infra-Low Frequency Neurofeedback Impact on Post-Concussive Symptoms of Headache, Insomnia and Attention Disorder: Results of a Randomized Control Trial, EXPLORE (2025),
https://doi.org/10.1016/j.explore.2025.103137
When VA scientists were first briefed on the results of the study earlier this year, they were impressed: “These results fall outside of the realm of our prior experience.” Nearly all the measures showed large effect sizes, and all changes in symptom severity were clinically significant. Nearly all the participants had a history of ten or more prior treatment failures over the course of more than ten years.
This controlled study was preceded by a pilot study on four trainees with combat-related TBI that also demonstrated stellar results (but unsurprising to those of us who have been engaged with the method over the years).
J. Carlson, G.W. Ross (2021). Neurofeedback impact on chronic headache, sleep, and attention disorders experienced by veterans with mild traumatic brain injury: a pilot study, Biofeedback, 49 (1) (2021), pp. 2-9, 10.5298/1081-5937-49.01.01
The most serious shortcoming of the above formal study is that the post-testing occurred after a mere twenty sessions of training. This is plainly insufficient for such a heavily impaired treatment population (nearly all were rated totally disabled by the VA). Ideally one would want to train until a plateau is reached, which almost surely would involve forty or more sessions for many. (Remarkably, one MD in the group was able to return to his professional work after the twenty sessions.)
A further limitation is that only a single protocol schema was used, whereas in the clinical world additional protocols would likely be recruited. Endogenous neuromodulation targets the self-regulatory competence with respect to core regulatory domains of arousal regulation, affect regulation, autonomic regulation, and interoception (the salience network). It also targets the stability of the nervous system against excursions into pathological states such as migraines, flashbacks, rage, or the sudden impulse to suicide.
When the psychological aspects of the trauma response—moral injury, survivor guilt, or remorse—are at issue, we draw upon a different protocol altogether. This goes under the name of Alpha-Theta training. It was first brought to the attention of the neurofeedback community back in 1990, after its formal evaluation at the Fort Lyon Colorado VA in the remediation of PTSD-related alcoholism by psychologist Eugene Peniston. Participants in that first study all had a history of at least four prior treatment failures at the VA. All ten experimentals became abstinent (and remained so on follow-up over the years), while all the controls relapsed within two years. Peniston published two replications by 1993 that demonstrated comparable results. In the second study, the formal target became PTSD rather than alcoholism, in recognition of the fact that the underlying issue was the PTSD, of which the alcoholism was a symptom. Ironically, these studies collectively evoked a lot of skepticism simply because the results were ‘too good to be true.’ Consequently, the work was ignored by the research community, and was only carried forward by clinicians.
Our clinic followed with the largest controlled study of drug addiction done to date, beginning in 1995, and involving 121 participants. It combined the Peniston Alpha-Theta Protocol (which had been developed and matured at the Menninger Foundation over the course of many years, starting in 1968) with beta-band training for physiological normalization and impulse control. It was a four-year study, including three-year follow-up. The addition of NF to the conventional addiction treatment (Minnesota Model) led to a factor of three improvement in relapse prevention at one year (nominally 75% versus 25%). At three years, the experimentals had retained their state of abstinence, while the controls had continued to relapse.
After a series of rejections over several years, the paper was published in 2005 in the American Journal of Alcohol and Drug Abuse:
Scott, W.C., Kaiser, D.A., Othmer, S., and Sideroff, S.I. (2005). Effects of an EEG Biofeedback Protocol on a Mixed Substance Abusing Population (2005). The American Journal of Alcohol and Drug Abuse, 31, 455 – 469 DOI: 10.108/ADA-200056807
It can be readily accessed on ResearchGate, where it is presently ranked at the 98th percentile in terms of Research Interest.
https://www.researchgate.net/publication/7600661_Effects_of_an_EEG_Biofeedback_Protocol_on_a_Mixed_Substance_Abusing_Population
In this study, we had achieved sobriety, but we had not systematically achieved recovery. Many were still subject to cravings, and remained sober through gritted teeth, and by dint of participation in the group experience of the 12-step program. Something more was needed….
The method of Endogenous Neuromodulation benefited over the years from a migration to the infra-low frequency domain from the more conventional EEG range where the technique was first developed. This came about by virtue of our discovery in the late nineties of the Optimal Response Frequency principle (ORF). These oscillators, distributed over the frequency spectrum, are responsible for organizing the entire frequency domain. The search for the ORF over a large client pool led to a strong dominance of the lower frequencies in the distribution. The tables were being turned. Instead of our training the brain on the basis of our wisdom, the brain was informing us about how it is best trained. Extending the training to ever lower frequencies eventuated in 2006 in the incursion into the infra-low frequency domain, below 0.1 Hz.
This favors the training of core state regulation, which is organized in the frequency range of interest in fMRI research, 0.1 to 200 mHz. Clinical results were better across the board. There was no going back. By now, this method is in the hands of some 8,000 clinicians in forty countries, and more than a million people have already benefited from the training at their hands. The method is quite well established in the clinical realm.
The payoff in the recovery from PTSD, TBI, depression and addiction soon became apparent. Our method was introduced into the Salvation Army Bell Shelter in 2008. There we experienced what we took to be a miracle story with their most challenging resident. This is written up as a newsletter that can be accessed here: https://news.eeginfo.com/recovery-from-ptsd-a-vietnam-veteran/. This experience led to a scaling up of the operation at Bell Shelter in 2009, where it was utilized mainly in application to formerly homeless Vietnam era veterans. A video made by the Salvation Army can be seen here: https://youtu.be/t-5metrcUA4.
This also led to the establishment of our non-profit venture, Homecoming for Veterans, under which veterans could receive care at no cost with participating network practitioners (www.homecomingforveterans.org)
The first publication based on the infra-low frequency training in application to PTSD appeared in 2009:
Siegfried Othmer and Susan F. Othmer (2009), Post-Traumatic Stress Disorder—The Neurofeedback Remedy, Biofeedback, 37(1), pp. 24–31
It is accessible here: https://www.researchgate.net/publication/239280365_Post_Traumatic_Stress_Disorder-The_Neurofeedback_Remedy
In 2008, I had the opportunity to present our work at a Combat Operational Stress Control Conference in San Diego. That led to the introduction of our method at Camp Pendleton in 2009, where it became the therapeutic remedy of choice at the Department of Deployment Health. All their clinical staff was trained in the method, and it remains in use to this day at the Department of Mental Health.
Outcomes of the first 300+ service members were tracked, and the results can be seen in the following Dropbox file:
https://www.dropbox.com/scl/fi/dphfzbdfhspso62kqgdxw/Comprehensive-Summary-of-PTSD-data-as-of-Jan-2011-6-20-24.pdf?rlkey=dh1l2citrzr0vwj5sdrcyufs6&dl=0
Results were presented in four presentations at a Combat Operational Stress Conference in 2011. Three of these were mine (on PTSD, Sleep, and Resilience), and one was by staff members from the Department of Deployment Health.
Villanueva, M., Benson, A., LaDou, T. Clinical practice and observations of infralow neurofeedback as an adjunctive treatment within Camp Pendleton’s Deployment Health Center. NCCOSC conference, April 2011.
The results were also written up for presentation to Dr. Antonette Zeiss, Deputy Chief Consultant, Mental Health Services for the VA, in Washington, DC, in 2011:
Psychological Health and Neurofeedback: Remediating PTSD and TBI (2012) Siegfried Othmer DOI:10.13140/RG.2.2.36316.81288
This comprehensive coverage of the topic is readily accessible here: https://www.researchgate.net/publication/380291048_Psychological_Health_and_Neurofeedback_Remediating_PTSD_and_TBI
We also made contact with Matthew J. Friedman, Executive Director and Head of Research at the National Center for PTSD in White River Junction, Vermont. Dr. Friedman consulted his academic colleagues, and on that basis rejected any overtures from our camp. We were now totally blocked from moving forward within the VA. The Boston VA had gone so far as to purchase $100K of instrumentation, and it was all just put on the shelf. We taught many professionals from the West Los Angeles VA at no cost in order to get buy-in, and then they were not allowed to put their new competence into practice.
It was also in 2011 that an appeals court ordered the VA to overhaul mental health care. From the Associated Press:
Noting that an average of 18 veterans a day commit suicide, a federal appeals court Tuesday ordered the Department of Veterans Affairs to dramatically overhaul its mental health care system.
In the strongly worded ruling, the 9th U.S. Circuit Court of Appeals said it takes the department an average of four years to fully provide the mental health benefits owed veterans. The court also said it often takes weeks for a suicidal vet to get a first appointment.”
The “unchecked incompetence” in handling the flood of post-traumatic stress disorder and other mental health claims is unconstitutional, the court said.
“No more veterans should be compelled to agonize or perish while the government fails to perform its obligations,” Judge Stephen Reinhardt wrote for the three-judge panel.
In this adverse environment the relevant officials in charge of research decided to ignore a potentially efficient remedy not only for PTSD generally, but for depression and suicidality, specifically.
The method was introduced at Fort Hood in about 2011, and it was adopted by several other military bases during the time of major deployment. The method was also introduced into Iraq and into Afghanistan (forward operating base Spin Boldak), where it was utilized in an optimal functioning frame and PTSD was not usually an issue. Taking advantage of both ILF NF and Alpha-Theta became routine for the men on base, including the command staff and medical personnel. The supervising clinician was Major Michael Villanueva, who had gotten his sea legs in ILF NF at Camp Pendleton originally and was also responsible for introducing the method at Fort Hood.
In 2014, the Swedish Red Cross in Malmö performed a pilot study on ten trauma victims from the Middle East wars for ten sessions. Outcomes were promising, but more sessions were needed.
In 2016, the Swedish Red Cross in Stockholm performed a second pilot study, this time for twenty sessions. Excellent results were obtained, but quite obviously twenty sessions were not sufficient either.
Can Neurofeedback reduce PTSD symptoms in severely traumatized refugees? Frida Johansson Metso, Dipl. Psychologist, Assistant Director Karin Duberg, MD. Psychotherapist. (I would be happy to furnish the text of the unpublished report.)
In 2020 a Swedish practitioner published a case report on a refugee with complex PTSD that involved both sexual trauma and war-related violence. Full resolution was achieved in only ten training sessions. Such rapid recovery was unprecedented in our experience, but it illustrates what is possible even in the most horrid of life histories.
Anna Gerge (2020). A multifaceted case-vignette integrating neurofeedback and EMDR in the treatment of complex PTSD, European Journal of Trauma & Dissociation 4 (2020) 100157
https://doi.org/10.1016/j.ejtd.2020.100157
I wrote a newsletter about this study, which is accessible here: https://news.eeginfo.com/a-case-of-ptsd-and-dissociative-identity-disorder/
The lead researcher in the latest study at the VA Pacific Islands Health Care System, Dr. Judy Carlson, had a nearly quarter century of experience with the method before she managed to obtain VA funding for this study in 2019. Given the prevailing foreclosure of further research opportunity within the VA, Dr. Carlson has decided to retire. The risk exists that, in consequence, this promising research will not have an opportunity to bear fruit within the VA.
This method is ready for prime time. Thousands of service members and veterans have already benefited over the past seventeen years. Without question we have here an opportunity to restore our veterans to functionality at low cost and in short order. The typical program cost of neurofeedback would likely range from $7,000 to $10,000 per trainee, with enormous positive fallout for the individual, for the family, and for the larger society.
Let us not fail to seize this opportunity within the VA once again, despite any distractions from the psychedelics coming into the picture. The psychedelics give us a glimpse of what is possible with non-pharmacological remedies. ILF NF plus Alpha-Theta training are the systematic means of getting to recovery, and ultimately to optimal functioning.
Siegfried Othmer, Ph.D.
Chief Scientist, The EEG Institute
Board Chair, The Brian Othmer Foundation
Los Angeles
www.brianothmerfoundation.org
www.eeginfo.com
www.eeginstitute.com
www.homecomingforveterans.org
P.S. When I went down to Camp Pendleton to brief the staff on the results for the first 300+ trainees in 2010, a Marine was sitting in the waiting room hoping to talk to me. He did not get the chance. When we emerged from the briefing some 90 minutes later, he was still there. With an emotional tone, he simply had to tell me personally just how transformative the training had been for his life. As I am not a practitioner myself, this moment is etched in my permanent memory.
A medical practitioner at a medical conference in 2023: “I am in awe of what I can accomplish with Infra-Low Frequency Neuromodulation.”
Mark A. Reger, PhD, US Department of Veterans Affairs, 9600 Veterans Dr SW, 116-R, Tacoma, WA 98493 (Mark.Reger@va.gov).
Re: Mental Health Research in the Department of Veterans Affairs
Mark A. Reger, PhD; Miriam J. Smyth, PhD





