Recovery from PTSD: A Vietnam Veteran
by Siegfried Othmer | February 19th, 2009 We have just experienced a remarkably quick recovery from PTSD symptoms in a Vietnam veteran. The case is illustrative of the more rapid pace of recovery that is achievable with the latest neurofeedback techniques that encompass the infra-low range of EEG frequencies. The veteran has had a forty-year history of PTSD, and was rescued from homelessness by the Salvation Army here in Los Angeles. He came to our offices for intensive neurofeedback training through the auspices of the Salvation Army. In exchange for our providing services at no cost, the veteran has allowed us to make his case history available for the benefit of other clinicians.
We have just experienced a remarkably quick recovery from PTSD symptoms in a Vietnam veteran. The case is illustrative of the more rapid pace of recovery that is achievable with the latest neurofeedback techniques that encompass the infra-low range of EEG frequencies. The veteran has had a forty-year history of PTSD, and was rescued from homelessness by the Salvation Army here in Los Angeles. He came to our offices for intensive neurofeedback training through the auspices of the Salvation Army. In exchange for our providing services at no cost, the veteran has allowed us to make his case history available for the benefit of other clinicians.
For scientific purposes, the veteran has agreed to undergo pre-post quantitative EEG analysis (courtesy of QMetrx) and SPECT imaging (courtesy of the Amen Clinics). As the training is still on-going, these pre-post comparisons are not yet available. However, we do have initial symptom-tracking data that already tell quite a story. Symptoms are assessed on the basis of self-report at typically three-session intervals. Severity is rated on a ten-point scale. Results for the first eighteen training sessions are shown in Figure 1. Overall symptom reduction reached 50% by session ten, and was more than 80% by session eighteen. The symptom list was broadly inclusive, and covered a number of areas not considered to be classically associated with PTSD. Eleven out of the twenty major symptoms were rated at zero by session 18. None were rated higher than 4 out of ten by session 18. The picture is one of broad improvement in self-regulatory capacity.
The picture is actually even more dramatic when data are segregated for the symptoms commonly associated with PTSD. These are shown in Figure 2. With regard to PTSD symptoms, overall improvement reached 50% within three sessions, and reached 93% in 18 sessions. Even more significantly, nightmares, flashbacks, suicidal thoughts, and binging and purging were all eliminated within three sessions. These were the most troublesome PTSD-related symptoms. The most persistent symptoms related to the quality of sleep. At the first QEEG session it became obvious that the veteran was suffering from sleep apnea. He was unable to stay awake for the QEEG assessment. This was a problem during the early neurofeedback sessions as well. By session 18, he was getting through entire alpha-theta sessions without falling asleep. Other persistent symptoms relate to motor function and mobility. Currently the veteran remains confined to a wheelchair. The improvement in hypertension is not entirely attributable to neurofeedback: as a result of the training, the veteran was motivated to be more consistent in taking his blood pressure medication.
Figure 1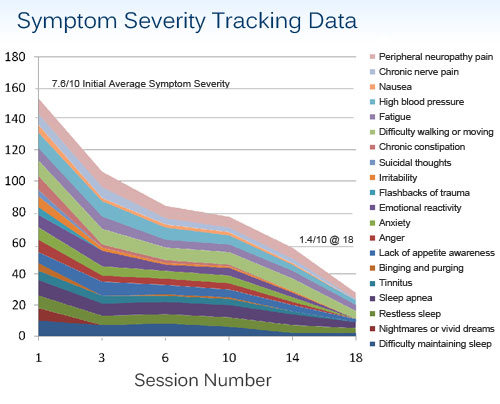
Figure 2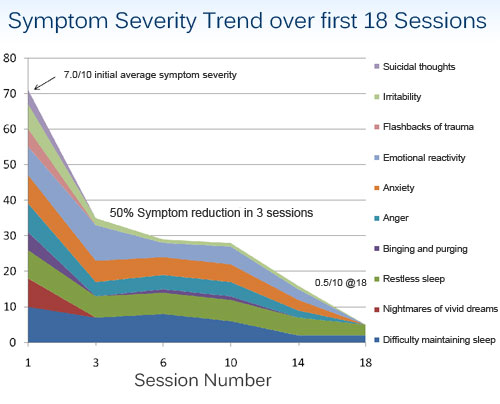
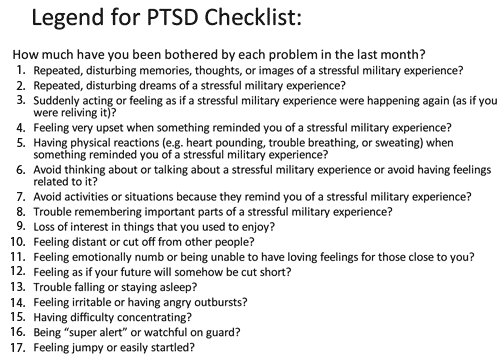
Ratings for a military standard PTSD checklist are also available, and are shown in Figure 3 for comparison of pre-training values with those after session 19.
EEG training is continuing, but the focus is shifting toward alpha-theta training in order to allow the veteran to come to terms with the extraordinary life changes that he is now undergoing. He remains in a fragile state, full of ambiguity regarding his future. The remaining symptoms no doubt call for longer-term training: sleep quality; mobility and motor control; peripheral neuropathy pain (secondary to diabetes). But the focus will increasingly shift toward functional augmentation and away from symptom reduction.
The veteran was trained with our standard set of single-channel bipolar protocols, using reinforcement at the optimum reward frequency (ORF), combined with multiple inhibits.
The migration to infra-low frequencies is not an arbitrary choice on our part but rather is dictated by the response to the reinforcements. However, in nearly all cases of PTSD the ORF appears to fall within the infra-low range of frequencies, i.e. below 0.1 Hz. The selection of the optimum reward frequency is critical to success in this process, and even seasoned neurofeedback clinicians are strongly cautioned not to undertake this training casually or without proper professional training in this particular method.
The rapid response of PTSD to this straight-forward neurophysiologically-based technique supports the case for neurofeedback as a primary intervention for PTSD, leaving the cognitively-based and psychodynamic therapies for a later role as the person attempts to reconstruct his or her life. When this case is placed in the context of similar such cases in our clinical experience, we have a demonstration here of a benign alternative to exposure-based therapies and other labor-intensive, extended therapies to effect recovery from the symptoms of PTSD. Recovery is also much more comprehensive than would be expected with any psychologically-based technique, including EMDR. The report also demonstrates that the duration of symptoms (40-some years in this case) does not stand in the way of effecting substantial recovery, nor does the extremity of initial symptom severity. This case, among others, holds out significant hope for the large number of Vietnam veterans who still suffer from PTSD to this day.
Figure 3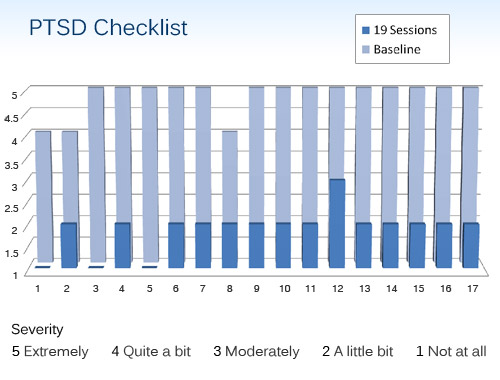
It is particularly heartening that with this training the suicidal ideation ceased almost immediately. We have just recently crossed the threshold at which more Vietnam veterans have been lost to suicide since the war than we had war casualties in theatre. The potential for improving the quality of life of our remaining Vietnam veterans through neurofeedback is immense.
In this regard, it is also significant that we are coming to this task with an entirely new approach. By now the typical Vietnam veteran is quite settled in terms of expectations for his future, and no doubt brings a healthy skepticism to any invitation to further “therapies.” Neurofeedback can be successfully promoted to such a skeptical audience because the focus is entirely on enhancing function. The elimination of symptoms is a side effect of the process of restoring functionality and wholeness. Although clinicians would obviously like to have a full picture of what they are up against, it is not even necessary for the vet to disclose all of what bothers him. The project can succeed entirely with a focus on enhancing the brain’s functional scope. No failures or shortcomings need to be acknowledged to qualify for neurofeedback. No personality issues need to be bored into. No blame needs to be placed or responsibility assigned. One simply trains the central nervous system to self-regulate, and the brain to perform better, in a manner that is unique to each nervous system.
With neurofeedback we can counter the hidden fear of many long-term disabled veterans that their symptoms are their indispensable lifeline to continued disability compensation. The realistic prospect of fully restored functionality must be in prospect, not mere symptom relief. With this veteran, we have passed only the first milestone. The second one remains.






Hello.
Is it possible to say or describe how you resonate to find the propper electrode placements in those cases? Thanks:)
C
Yes, it is possible to describe that process very specifically. We do so in our training course for professionals.
Fortunately, the beginning of the training tends to simplify greatly. Nearly all veterans have almost the same starting point to their training. It differentiates as time goes on, and as we find out what each nervous system requires.