Introduction to Infra-low Frequency Training
by Siegfried Othmer | March 10th, 2010 The first convincing evidence for EEG feedback efficacy in the management of pathophysiology was with regard to generalized seizures. The early work by Sterman, Lubar, as well as the subsequent follow-up by others, therefore remains a crucial point of reference for the various feedback techniques that have built upon the early protocol of SMR reinforcement combined the theta-band and high-beta band inhibition. Remarkably, the essential features of the early approach have been retained in the various evolutionary pathways that have emanated from the early work. This essential similarity has perhaps obscured other aspects of the training approach that have changed substantially over time, the significance of which may not have been fully appreciated except in reflection. In this newsletter we consider some of these changes and their implications generally, as well as for seizure management in particular.
The first convincing evidence for EEG feedback efficacy in the management of pathophysiology was with regard to generalized seizures. The early work by Sterman, Lubar, as well as the subsequent follow-up by others, therefore remains a crucial point of reference for the various feedback techniques that have built upon the early protocol of SMR reinforcement combined the theta-band and high-beta band inhibition. Remarkably, the essential features of the early approach have been retained in the various evolutionary pathways that have emanated from the early work. This essential similarity has perhaps obscured other aspects of the training approach that have changed substantially over time, the significance of which may not have been fully appreciated except in reflection. In this newsletter we consider some of these changes and their implications generally, as well as for seizure management in particular.
The common thread in most modern neurofeedback approaches is the combination of a reinforcement strategy on one EEG frequency or another and an inhibit strategy based on detection of excursions into dysregulation. Some issues relating to the inhibit side have been relegated entirely to the software, thus removing them from ready visibility. Artifact detection and the division of labor between that and the conventional inhibits is a case in point. Specific targeting strategies typically remain to the discretion of the practitioner, as for example with respect to thresholding, placement, and frequency band selection. The general thrust over time has been to broaden the “field of view” of this EEG-based disregulation detector, mainly with respect to the frequencies being targeted, but sometimes also in terms of placement. Multi-channel instruments allow independent choice of placement for the reward and the inhibit strategies. Fortuitously, the various inhibit strategies being actively used—-though differing significantly from each other—-have not been wrapped up in much controversy.
Far more discretion prevails with regard to the reward strategy, and unsurprisingly most of the proliferation of alternatives, and hence most of the unresolved issues in the field, relate to that aspect of the protocol. In the early work, the discrete detection of an SMR bursting response in cats, combined with discrete rewards, firmly established that operant conditioning of the EEG could be routinely achieved. In the subsequent training of human subjects, the dollop of food reward was replaced by a mere beep tone. More significantly, the waking human EEG did not typically exhibit the distinct SMR bursting response that could be seen in cats. The distribution of SMR amplitudes was instead well-behaved. With a continuous, quasi-Gaussian amplitude distribution, the choice of threshold was left somewhat arbitrary, whereas in cats the threshold level had been largely dictated by the double-humped distribution. Given the separation between the background EEG amplitude distribution in the SMR band and the distribution in bursting amplitudes, a threshold could always be selected that would discriminate the bursts unambiguously.
In the clinical setting, as distinct from the research setting, a second feedback loop is always operative, namely on the clinician monitoring the feedback process of the client. As it happens, the behavior of early clinicians was gradually shaped to offer rewards more generously than had been the case for the underlying research. This was done through easing the reward threshold. By way of contrast, both Sterman and Lubar had maintained high thresholds in order to discriminate the rare, large excursions in SMR burst amplitude. The reward incidence was correspondingly low, by analogy to what had transpired in the cats. With the emergence of more generous thresholding, the discrete reward (beep tone) eventually became so plentiful that hearing it became an expectation. The dropout of the tone became the ‘odd-ball’ event to which attention would be preferentially devoted, the reverse of what had originally been intended, and the reverse of what had been done in the original research.
The discrete reward had come to function like an inhibit. On the other hand, in terms of clinical results the reward functioned just as it had before. If anything, the training had become even more efficient with the relaxation of the reward criteria. The mystery was resolved with the realization that the principal source of information to the client lay in the accompanying continuous information flow on the instantaneous reward amplitude. The beeps had been reduced to mere accompaniment for most sighted individuals.
Years later Sterman appealed to the neurofeedback community that in the spirit of learning theory one ought to allow a sufficient refractory period between discrete rewards to permit consolidation, but by the time he forcefully put this forward the die had already been cast, and most practitioners were using instrumentation that implemented the new regime. The emphasis had shifted toward the analog reward signal as the bearer of the principal burden of the feedback. There had to be a heightened information density to explain the quicker responses of trainees, and the rapidly fluctuating analog signal was the only explanation.
It has largely gotten lost in the flow of subsequent developments that both Sterman and Lubar used bipolar montages in all of their early research on human subjects. In our work we used both bipolar and referential montages, and a general impression emerged that the bipolar montages yielded stronger effects. This could, however, also have been due to placement. One could never be sure. Confirmation of sorts was provided subsequently by the general observation that two-channel coherence training is typically more powerful than referential amplitude training. Both bipolar placement and two-channel coherence training weight the relative phase of activity at the two sites more heavily than referential training, which involves us directly in the issue of connectivity. This follows from the observation that if the reference were entirely neutral, then phase would not enter the picture at all. In between, we are on a continuum.
Additionally, it was observed that clients differed in their response to particular reward frequencies, and that their clinical response could be optimized by small adjustments in the reward frequency. In some instances, small adjustments became large adjustments, and eventually this approach could no longer realistically be referred to as SMR-training. Remarkably, however, the optimal reward frequency (ORF) for a client was largely unrelated to the underlying clinical condition. And just as SMR-training had come to serve a variety of objectives having little or nothing to do with the motor system specifically, the optimized training was if anything even broader in its clinical impact.
At one of our training courses, an attendee who remained to be persuaded was watching a demonstration of the optimization procedure on a volunteer from the class, his critical faculties on high alert. As the trainee reported changes in alertness, in feelings, and in symptom severity after mere minutes, the skeptic exclaimed: “This cannot be operant conditioning!” And he was right. Significant learning cannot have been accomplished on this time scale. All we had really done is to shift the client’s state in the moment. Still, that required a lot of information, which only the analog signal was capable of providing. The analogy here is to traditional biofeedback, where attending to analog GSR and temperature signals in first instance simply induces state shifts. The learning of new behavior is then the consequence of numerous repetitions.
The Trend toward Infra-low Frequency Training
In the continuing exploration of the optimization procedure with each client, it was observed that we often bumped up against the lower limit of the frequency range that our software provided for. Early on, we allowed for reward-based training down to 4-7 Hz. (Three-Hz bandwidth was standard for the reward band.) Over time it became clear that many clients were bumping up against the lowest frequency, and one had the impression that many needed to train even lower. When the software was extended down to 0-3 Hz, the distribution changed further, and revealed the lowest center frequency, 1.5 Hz, to be the most populated. Again one had the impression that some clients needed an even lower reward frequency. When the software was further extended to allow operation down to 0.1 Hz cutoff frequency, over time the center frequency of 0.05 Hz became the modal value. The same occurred when we extended the range down to 0.01 Hz in center frequency. And finally we extended the range to the ‘absurd’ value of 0.001 Hz in November 2008. The lower range that had been opened up immediately became populated, and once again the modal value became the lowest we had available, 0.001 Hz.
Looking over the past year of clinical experience in our office, 77% of all clients optimize their response at the lowest frequency (129/167), and 90% optimized below 0.01 Hz (151/167). The distribution is shown in Figure 1. Observe that the abscissa scales logarithmically in decades per division, but within each division the scale is linear. As our current experience is compared with the earlier “trials” with higher cutoff frequencies, an interesting pattern emerges. As we went down in minimum cutoff frequency through all of the stages listed above, the distribution became ever more skewed in favor of the lowest frequency rather than less. This is contrary to what one would expect. One would have expected the equivalent of unrolling a carpet, gradually exposing more of the pattern of nature as the software progressively made this possible. But in fact the whole distribution kept changing as we went. Note in this regard that in the current distribution the earlier peaks at 13.5 Hz (the 12-15 Hz SMR band) and 16.5 Hz (the 15-18Hz low beta region) are no longer discernible, nor are the subsequent peaks of (successively) 5.5 Hz (4-7 Hz band), 1.5 Hz (0-3 Hz band), 0.05 Hz, and 0.01 Hz.
Figure 1 shows the distribution in optimum reward frequencies observed in 167 clients seen in our office during 2009. Figure 1a shows the full distribution; Figure 1b shows the same data on a finer scale. The abscissa scales logarithmically in decades per division, but within each division the scale is linear. The plot is therefore best seen as a concatenation of several linear plots each covering a decade in frequency. The strong dominance of the lowest available reward frequency of 0.001 Hz is apparent. This data point is truncated in Figure 1b.
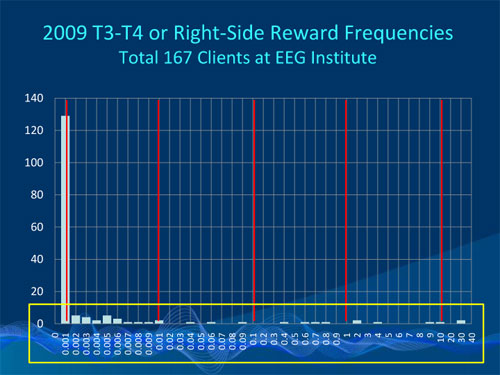 Figure 1a
Figure 1a
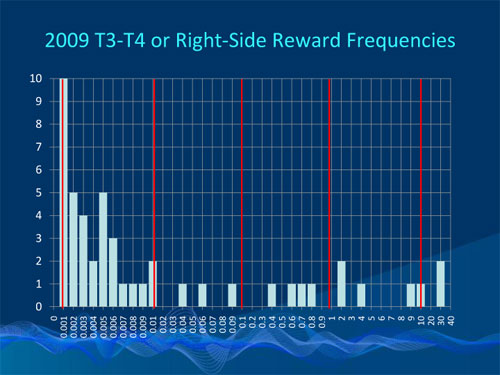 Figure 1b
Figure 1b
At the top level one must assign the changing distribution to our clinical learning curve. It took us years to become fully conversant with this new frequency domain. But more specifically it also became very clear that the training was stronger at the lower frequencies, and correspondingly more frequency-specific. The more deeply we penetrated into the ILF range, the more precision was called for in the choice of reward frequency. Reflecting back on our earlier history from our current perspective, it is apparent that optimal frequency training was not available for some 90% of our clinical population even as we were finding our way with the optimum reward frequency model. All we were in a position to accomplish along the way was a kind of ‘local optimization’ that should not be expected to reflect the distribution once global frequency optimization became a possibility.
The Clinical Role of ILF Training
The defining characteristics of the protocol are bipolar placement and optimization of the reward frequency without restriction (combined, of course, with an inhibit strategy). However, since over 90% of all our clients optimize in the ILF range, and since novelty attaches to that aspect specifically, this training approach has come to be referred to as ILF training as commonly as ORF training. The frequency-optimized bipolar training has unambiguously improved our outcomes across the board with our clinical population, and this includes in particular medically refractory seizures, which remain a benchmark for comparison purposes across the decades.
Our challenge is to provide a theoretical framework in which these results may be understood. The bipolar placement can be seen as having a bias toward network desynchronization, which in turn is thought to be intrinsically stabilizing in the case of seizure susceptibility. This could equally have been the operative mechanism in Sterman’s and Lubar’s classic papers in which bipolar placement was used. On the other hand, the target in the cat work was clearly network synchronization in the SMR band. These disparate approaches, both leading to a common end result, can be reconciled by thinking of certain protocols in terms of setting up challenges as opposed to prescribing destinations. After all, neither network synchronization nor desynchronization represents a desirable steady-state condition.
It is helpful in this regard to draw on the collective wisdom from our sister disciplines of peripheral biofeedback. Even in temperature training, where a clinical objective was unambiguous, clinicians often relied upon alternating up- and down-training. The immediate objective was enhanced control. Peripheral biofeedback also helps us to understand working in the ILF region. Here we are tracking the slow cortical potential through its (differential) migrations on very long timescales. Threshold crossings in the traditional sense are extremely rare at the lowest frequencies. Much can happen between one threshold crossing and the next, so the threshold can no longer be critical to the proceedings. It has become entirely a matter of process, and that’s where traditional biofeedback has already been—-for example with Heart Rate Variability (HRV) training. Merely by focusing on the instantaneous beat-to-beat interval, the trainee affects the entire HRV spectrum, all the way down to the ILF range.
The journey has become much more important than the destination. Goal setting has become less relevant. The idea of discrete rewards has lost meaning in this context. Rather, the watchword now is engagement with the process. Engagement here refers to the brain rather than to the client, and in practice this means the brain must recognize its agency with respect to the proffered signal. Such recognition is obviously favored by a continuous rather than episodic signal stream.
Now when it comes to promoting engagement, we seem to be better off at the optimized reward frequencies in general, and at the infra-low frequencies in particular. At first glance this seems entirely counter-intuitive because in the ILF range we have much less ‘information density’ to convey back to the client than we do in the SMR/beta range, where the training can be highly dynamic. There must be a compensating factor, and it is likely that the ILF region ties us in much more directly to the core regulatory functions of arousal regulation, affect regulation, autonomic regulation, and interoception that are foundational for our enterprise. Even more fundamentally, it is necessary for the regulatory system to maintain unconditional stability, and in this regard the ORF training has been a clear step forward in our clinical experience.
It is not only our experience with seizures that testifies to this. Indeed, we have not yet seen many seizure cases in the 400 or so days since we’ve had the 0.001 Hz capability available to us. The proposition is also supported by our experience with other brain instabilities such as migraine, panic attacks, vertigo, episodic tinnitus, rage behavior, and Bipolar Disorder, all of which respond nicely to ORF training with the same placement we use for seizure management.
It is tempting to suggest that a kind of ‘hierarchy of needs’ applies to neurofeedback, one in which brain stability is the paramount issue, and in which the foundational regulatory mechanisms should be normalized before one addresses higher-level issues. The latter include specific learning disabilities, specific sensory processing deficits, working memory, and any localized deficits such as those attendant to organic brain injury, all of which may benefit selectively from highly targeted, QEEG-guided training.
At the outset above a distinction was made between merely evoking state shifts and actually acquiring learned control. As the technique gained in effectiveness over time, this distinction has become blurred. Mere state shifts can effect major enhancements to functionality and to the brain’s capacity for self-regulation. This means that one cannot use this method on a ‘set-and-forget’ basis. Constant vigilance on the part of the clinician is required in sensitive responders and in unstable nervous systems, in order to maintain optimization of the reinforcement parameters and to guide the process to the most propitious outcomes.
The method shapes the available brain plasticity in real time within each session, so the target of our exertions is always moving. A corresponding level of attentiveness is obviously required in connection with seizure disorder in particular, so this method should not be casually deployed. If the reinforcement parameters are not matched to the situation the person may be further moved into dysregulated states, giving rise to adverse effects which are characteristic of that particular nervous system. Unsurprisingly, this can be problematic as clinicians first encounter such a powerful method. It is therefore advisable for practitioners newly adopting this approach to get specialized training and to establish a consultative relationship with a seasoned practitioner.
In important ways we have come a long way from the early days of SMR training, and yet a basic kinship remains with the early seminal work that launched this field. At the same time, we may be re-establishing a kinship with peripheral biofeedback that has been lost along the way.
Reference:
Phase Sensitivity of Bipolar EEG Training Protocols
John A. Putman and Siegfried Othmer
Journal of Neurotherapy, 10(1), p.73-79 (2006)
Additional Resources:
Post-Traumatic Stress Disorder—The Neurofeedback Remedy
Siegfried Othmer and Susan F. Othmer
Biofeedback, 37(1), 24-31 (2009), AAPB
eeginfo.com/research/articles/PTSD-NeurofeedbackRemedy.pdf
Neuromodulation Technologies: An Attempt at Classification
Siegfried Othmer
In Quantitative EEG and Neurofeedback, Second Edition, Budzynski, Budzynski, Evans, Abarbanel, editors, Academic Press, San Diego (2009)
eeginfo.com/research/researchpapers/Neuromodulation_Technologies.pdf
Infra-low Frequency Training
Siegfried Othmer and Susan F. Othmer
eeginfo.com/research/articles/Infra-LowFrequencyTraining.pdf
Protocol Guide
Susan F. Othmer
eeginfo.com/shop/product_info.php/products_id/47





